 |
|
#196
|
||||
|
||||
|
Re: Sexual Health News
What to know about micropenis
https://www.medicalnewstoday.com/articles/323811.php Micropenis refers to an abnormally small penis. Micropenis is rare and hormonal or genetic issues are most often the cause. Doctors will usually diagnose and treat the condition at birth. In this article, we look at the definition of micropenis, the symptoms and causes, and the ways a smaller-than-average penis may or may not affect sexual and other functions. What is micropenis? Doctors diagnose micropenis when a person's penis is 2.5 standard deviations below the average stretched length for their age and level of sexual development. Research has estimated that the average penis size for an adult is 13.24 centimeters (cm) or 5.21 inches when stretched. For adults, doctors consider micropenis for a stretched penile length of less than 9.3 cm or 3.66 inches. When a person has micropenis, their internal genitalia and testicles are usually normal. Clinical sources define average and micropenis sizes for each age range, as follows: 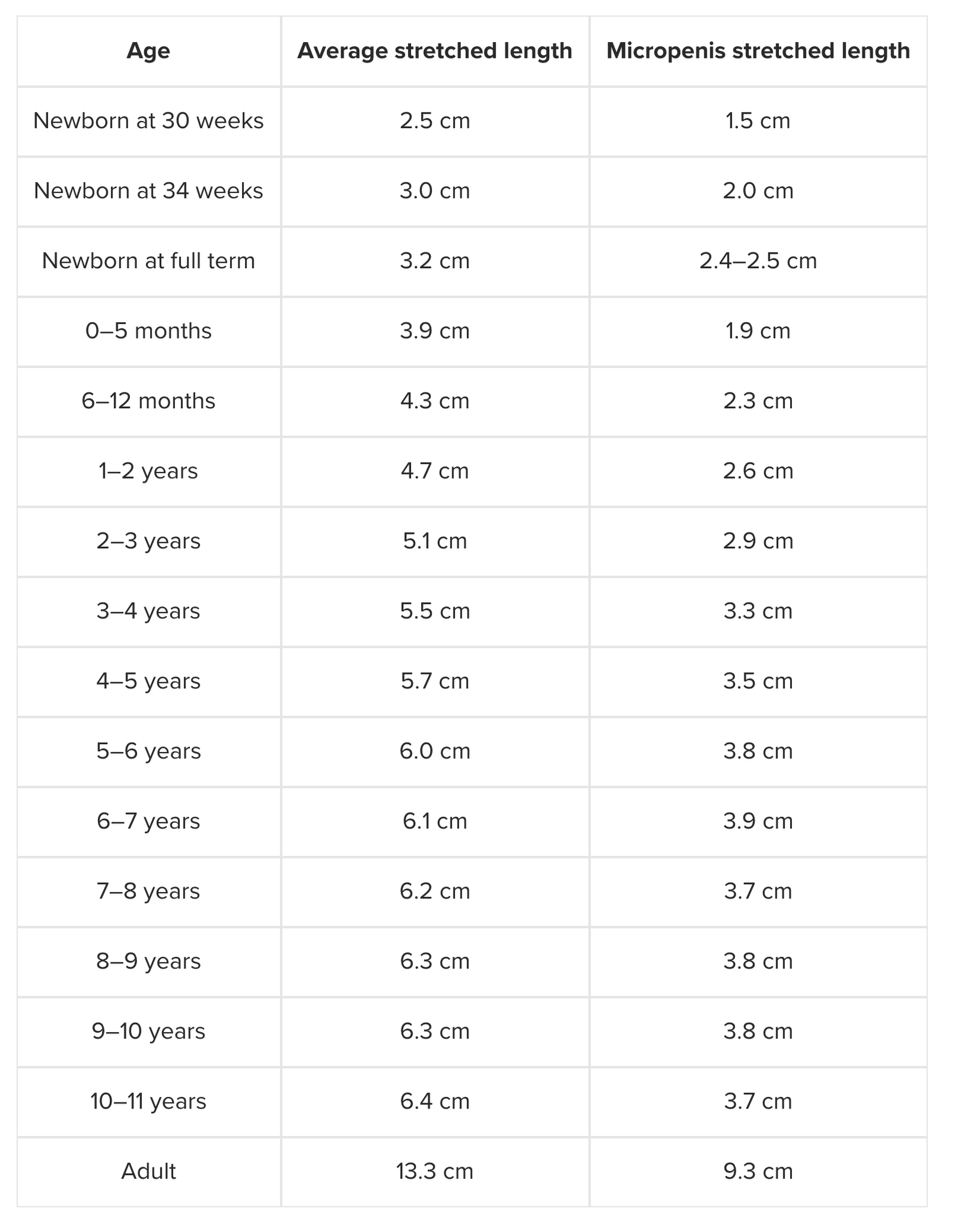 How common is micropenis? Micropenis is a rare condition that may affect around 1.5 in 10,000 male newborns, or 0.015 percent of male newborns in the United States, according to estimates taken between 1997 and 2000. The prevalence statistics of micropenis vary between studies. Micropenis and other birth abnormalities can be related to environmental factors, such as parental exposure to pesticides during pregnancy. As a result, this condition may be more common in specific populations. Causes Hormonal issues are the most common cause of micropenis. Less commonly, micropenis and other birth abnormalities can occur when the mother experiences exposure to pesticides or other toxic chemicals during pregnancy. Testosterone deficiencies, during pregnancy, are usually the cause of micropenis and may also cause other genital abnormalities. A testosterone deficiency can arise when a male fetus does not produce enough testosterone, or when the mother does not produce enough human chorionic gonadotrophin (hCG) hormone during pregnancy. hCG stimulates testosterone development in the fetus. When testosterone levels are normal, some medical conditions can stop a person's body from responding to testosterone correctly. This response is called androgen insensitivity. When any of these hormonal issues arise, the penis of a male fetus may not develop in the usual way. A male baby will experience a surge of testosterone around 0–3 months after birth. This is a crucial period for penile growth. If this process is interrupted by hormonal problems, a baby may have a smaller penis. In rare cases, micropenis is idiopathic, which means that a doctor cannot find a specific cause. Because hormone issues typically cause micropenis, people with this condition may have other symptoms, too. Some diagnoses that doctors may associate with micropenis include: hypogonadotropic hypogonadism Prader-Willi syndrome Kallmann syndrome growth hormone deficiencies abnormal chromosomes Laurence-Moon syndrome Sometimes what appears to be a micropenis is actually due to another problem. For instance, a baby born with swelling in the scrotum may look like they have a micropenis. The penis may also be less visible because of large surrounding fat pads when it is called buried penis and can occur in people with obesity. How does someone know if they have micropenis? Many people worry about penis size and typically think they are smaller than average even when they are not. If a person suspects they have micropenis, they may wish to see a doctor, who will be able to take accurate measurements and diagnose the condition. A doctor will usually diagnose micropenis at birth, however. If doctors suspect micropenis, they will measure the stretched length of the baby's penis and check for other signs of hormonal abnormalities. If a newborn's penis is abnormally small, a doctor may perform tests to assess the cause, including: Physical exams: Alongside measuring the penis, a doctor may look for other signs, such as unusual fat pads or growths. Blood tests: These can help the doctor check the baby's hormone levels. Doctors may also conduct genetic tests to determine the baby's biological sex. In rare cases, a baby who seems to have a micropenis may be intersex or have a sex chromosome abnormality. Imaging scans: A doctor may use imaging tests, such as a pelvic ultrasound or an MRI scan, to see the genitals and surrounding structures. Several other conditions can make the penis appear smaller than usual and may be confused with micropenis. Some of these can happen after circumcision. Alternative diagnoses to micropenis include: buried penis, where a fatty pad hides the true size of the penis webbed penis, where there is extra skin connecting the scrotum and the penis trapped penis, where there is not enough skin surrounding the penis Treatments Treatments aim to increase the penis size to ensure a person has a fully functioning penis and that they feel confident. A doctor may recommend the following treatments for micropenis: Hormone therapy Testosterone treatments can often help the penis to grow. Applying testosterone cream to the genitals during infancy, or giving intramuscular testosterone injections can increase penis size. Testosterone treatments are more effective before puberty than later on. Doctors may consider that a good response to testosterone treatment is a 100 percent increase in the penis length or an adequate response as a 3.5 cm increase in length. Different hormone treatments may help, depending on the cause of micropenis, so it is important that a person gets an accurate diagnosis. Surgery If hormone treatments do not work, surgery may help. A doctor can put an implant into the penis, which may make it look larger than before. However, this surgery carries a high chance of complications. Does micropenis affect sexual function? Most people with micropenis have normal sexual functioning. Micropenis does not affect a person's ability to urinate, masturbate, or orgasm. Some people may find it more difficult to urinate standing up. Anxiety about penis size can be a barrier to enjoying sex with a partner. Men may remain unsatisfied with their appearance even with treatment, though research shows that many men have normal sexual identities and functioning. Even so, people may benefit from counseling or sex therapy. Sexual intercourse is just one of many ways to enjoy sex with a partner. If a person has difficulties with sexual intercourse, this does not have to be a barrier to sexual pleasure for men and their partners. According to research from 2018, just 18.4 percent of women can orgasm with vaginal penetration alone Focusing on other sexual techniques, such as oral sex, may help a person feel more confident about sexual interactions, which can be a positive for both sexual partners. Outlook Micropenis is a condition where the penis is 2.5 standard deviations shorter than the average stretched penis length for a person's age. Testosterone deficiencies during pregnancy can cause micropenis. Less commonly, genetic abnormalities or environmental conditions can cause the condition. Micropenis is usually diagnosed and treated in infancy. Testosterone treatments in childhood show good outcomes. A person with micropenis may not obtain an average-sized penis, but this does not usually affect sexual functioning and identity. A wide range of penis sizes is normal. People with smaller-than-average penises can still have healthy, active sex lives. Counseling and sex therapy can help people to overcome anxieties about penis size or sex. |
|
#197
|
||||
|
||||
|
Re: Sexual Health News
London HIV patient becomes world's second AIDS cure hope
https://www.reuters.com/article/us-h...-idUSKCN1QL2C0 LONDON (Reuters) - An HIV-positive man in Britain has become the second known adult worldwide to be cleared of the AIDS virus after he received a bone marrow transplant from an HIV resistant donor, his doctors said. Almost three years after receiving bone marrow stem cells from a donor with a rare genetic mutation that resists HIV infection - and more than 18 months after coming off antiretroviral drugs - highly sensitive tests still show no trace of the man’s previous HIV infection. “There is no virus there that we can measure. We can’t detect anything,” said Ravindra Gupta, a professor and HIV biologist who co-led a team of doctors treating the man. The case is a proof of the concept that scientists will one day be able to end AIDS, the doctors said, but does not mean a cure for HIV has been found. Gupta described his patient as “functionally cured” and “in remission”, but cautioned: “It’s too early to say he’s cured.” The man is being called “the London patient”, in part because his case is similar to the first known case of a functional cure of HIV - in an American man, Timothy Brown, who became known as the Berlin patient when he underwent similar treatment in Germany in 2007 which also cleared his HIV. Brown, who had been living in Berlin, has since moved to the United States and, according to HIV experts, is still HIV-free. Some 37 million people worldwide are currently infected with HIV and the AIDS pandemic has killed around 35 million people worldwide since it began in the 1980s. Scientific research into the complex virus has in recent years led to the development of drug combinations that can keep it at bay in most patients. Gupta, now at Cambridge University, treated the London patient when he was working at University College London. The man had contracted HIV in 2003, Gupta said, and in 2012 was also diagnosed with a type of blood cancer called Hodgkin’s Lymphoma. LAST CHANCE In 2016, when he was very sick with cancer, doctors decided to seek a transplant match for him. “This was really his last chance of survival,” Gupta told Reuters in an interview. The donor - who was unrelated - had a genetic mutation known as ‘CCR5 delta 32’, which confers resistance to HIV. The transplant went relatively smoothly, Gupta said, but there were some side effects, including the patient suffering a period of “graft-versus-host” disease - a condition in which donor immune cells attack the recipient’s immune cells. Most experts say it is inconceivable such treatments could be a way of curing all patients. The procedure is expensive, complex and risky. To do this in others, exact match donors would have to be found in the tiny proportion of people — most of them of northern European descent — who have the CCR5 mutation that makes them resistant to the virus. Specialists said it is also not yet clear whether the CCR5 resistance is the only key - or whether the graft versus host disease may have been just as important. Both the Berlin and London patients had this complication, which may have played a role in the loss of HIV-infected cells, Gupta said. Sharon Lewin, an expert at Australia’s Doherty Institute and co-chair of the International AIDS Society’s cure research advisory board, told Reuters the London case points to new avenues for study. “We haven’t cured HIV, but (this) gives us hope that it’s going to be feasible one day to eliminate the virus,” she said. Gupta said his team plans to use these findings to explore potential new HIV treatment strategies. “We need to understand if we could knock out this (CCR5) receptor in people with HIV, which may be possible with gene therapy,” he said. The London patient, whose case was set to be reported in the journal Nature and presented at a medical conference in Seattle on Tuesday, has asked his medical team not to reveal his name, age, nationality or other details. |
|
#198
|
||||
|
||||
|
Re: Sexual Health News
10 ways to boost libido
By Zawn Villines https://www.medicalnewstoday.com/articles/323918.php Libido, or sex drive, naturally varies between individuals. Having a low sex drive is not necessarily a problem, but if a person wishes to boost their libido, they can try a range of effective natural methods. Anxiety, relationship difficulties, health concerns, and age can all affect libido. While a low libido is not usually problematic, it can affect a person's relationships and self-esteem. In this article, we look some of the best ways that males and females can increase their libido using natural methods. Natural ways to boost libido Both males and females can boost their libido using the following methods: 1. Manage anxiety Having high levels of anxiety is a common barrier to sexual functioning and libido for both males and females. This may be anxiety due to life stress or specific sex-related anxiety. People with an intense work schedule, caring responsibilities, or other life stresses may feel fatigued and, as a result, have a low sexual desire. Anxiety and stress can also make it more difficult for someone to get or maintain an erection, which can put a person off having sex. A 2017 review of erectile dysfunction in young men has suggested that depression and anxiety can result in a reduced libido and increased sexual dysfunction. There are many things that people can do to manage their anxiety and boost their mental health, including: practicing good sleep hygiene making time for a favorite hobby exercising regularly eating a nutritious diet working to improve relationships talking to a therapist 2. Improve relationship quality Many people experience a lull in sexual desire and frequency at certain points in a relationship. This may occur after being with someone for a long time, or if a person perceives that things are not going well in their intimate relationships. Focusing on improving the relationship can increase each partner's sex drive. This might involve: planning date nights doing activities together outside of the bedroom practicing open communication setting time aside for quality time with each other 3. Focus on foreplay Having better sexual experiences may increase a person's desire for sex, thereby boosting their libido. In many cases, people can enhance their sexual experiences by spending more time on touching, kissing, using sex toys, and performing oral sex. Some people call these actions outercourse. For women, foreplay may be especially important. According to some 2017 research, only around 18 percent of women orgasm from intercourse alone, while 33.6 percent of women report that stimulation of the clitoris is necessary for them to orgasm. 4. Get good-quality sleep Getting good sleep can improve a person's overall mood and energy levels, and some research also links sleep quality to libido. A small-scale 2015 study in women suggested that getting more sleep the night before increased their sexual desire the next day. Women who reported longer average sleep times reported better genital arousal than those with shorter sleep times. 5. Eat a nutritious diet Following a nutritious diet can benefit people's sex drive by promoting good circulation and heart health, and by removing specific foods that can decrease libido. Metabolic syndrome and cardiovascular disease can affect physical sexual functioning. Also, polycystic ovarian syndrome can affect hormone levels, which may also disrupt libido. Eating a diet rich in vegetables, low in sugar, and high in lean proteins can help prevent disorders that affect libido. 6. Try herbal remedies There is little research into how effective herbal remedies are at improving sexual function in males and females, though some people may find them beneficial. A 2015 review study states that there is limited but emerging data that the following herbal remedies may improve sexual function: maca tribulus gingko ginseng People should be wary of using herbal medicines without their doctor's approval. Some herbal medicines can interact with existing medications, and the Unites States Food and Drug Administration (FDA) do not regulate them. For this reason, their quality, purity, and safety remains unclear. 7. Maintain a healthful weight Some scientists link overweight and obesity to low sex drive, along with other factors related to reduced fertility. This is associated with hormonal factors, such as low testosterone concentrations. Some people who are overweight may also experience psychological effects, such as lower body confidence. Maintaining a healthy body weight can improve a person's sex drive, both physically and psychologically. Eating a healthful diet and getting regular exercise can help achieve this, as well as boost a person's overall energy levels. 8. Get regular exercise Getting regular exercise can help libido in many ways. A 2015 study of men undergoing androgen deprivation therapy, which lowers testosterone levels, found that regular exercise helped men cope with issues such as body image concerns, low libido, and relationship changes. A 2010 review of women with diabetes cites research showing that exercise may help lower diabetes-related symptoms in women. The study emphasizes that doing exercises of the pelvic floor may be useful in women without diabetes. 9. Try sex therapy Sexual desire is complex, with both psychological and physical components. Even when a person has a physical condition that affects libido, such as diabetes, improving the emotional and psychological response to sex can improve libido and sexual functioning. Therapy is an effective strategy for increasing low libido. Individual counseling can help address negative views about sex, self-esteem, and secondary causes of low libido, such as depression and anxiety. Relationship counseling can help some people work through factors affecting their sexual desire. Alongside talking therapies, mindfulness therapy may also help. One 2014 study found that just four sessions of mindfulness-based cognitive behavioral therapy in a group setting improved sexual desire, sexual arousal, and sexual satisfaction for women. To find a suitable therapist in your area, search the AASECT directory. 10. Quit smoking Smoking cigarettes can have a negative impact on a person's cardiovascular system. Good heart health is important for good sexual functioning. People who smoke cigarettes may find that their energy levels and sex drive increase after they quit. Boosting libido in males Libido in men is often related to testosterone levels, which will naturally decline as men age. Testosterone replacement therapy can help some men. In men with testosterone deficiency, or hypogonadism, testosterone replacement therapy can result in improved libido, reduced depression, and improved erectile function, according to one 2017 review. There is little evidence to suggest that certain foods or supplements increase a person's testosterone levels and sexual function. Some research suggests that zinc, vitamin D, and omega-3 fatty acids may be important dietary components for testosterone. Boosting libido in females Sex-related hormones, such as estrogen and estrogen-like compounds, can also affect sexual desire in females. Many women experience a dip in libido and sexual functioning at menopause, when estrogen levels drop. Estrogen replacement therapy may help some women. Vaginal dryness is another symptom of menopause. Using lubricants during sexual activity can increase people's enjoyment. Women also produce testosterone. Doctors once believed that testosterone might affect women's sex drive, but to date, research has not found a strong link. Certain birth control pills may also decrease libido. If a person suspects that their hormonal contraception is affecting their sex drive, they can speak with a doctor about changing pill type. When to see a doctor If a person is concerned about having a decrease in libido, a doctor can offer advice and information about potential causes and treatments. Doctors who are knowledgeable about alternative and complementary remedies may also help a person choose natural remedies. A person may wish to see a doctor for low libido when: it appears suddenly or without explanation additional symptoms appear, such as high blood pressure or pain it occurs after starting a new medication or having surgery it causes serious relationship problems or psychological distress sex is painful Summary There is a wide natural variation in people's sexual desires and libido. It is important to note that having a lower libido than other people is not necessarily a bad thing. However, if a person wants to increase their libido, there are many methods to try. These include eating a nutritious diet, getting regular exercise, reducing anxiety, and focusing on improving intimate relationships. Low libido is a complex issue, with relationship, psychological, and physical components. Knowing the cause can help a person find the best treatment. Because low libido, or a sudden shift in libido, can be a sign of a health condition, it is safest to talk to a doctor before trying libido boosters. |
|
#199
|
||||
|
||||
|
Re: Sexual Health News
What is female ejaculation?
By Amanda Barrell https://www.medicalnewstoday.com/articles/323953.php Female ejaculation is when a female's urethra expels fluid during sex. It can happen when a female becomes sexually aroused, but there is not necessarily an association with having an orgasm. Scientists do not fully understand female ejaculation, and there is limited research on how it works and its purpose. Female ejaculation is perfectly normal, although researchers remain divided on how many people experience it. In this article, we look at the current thinking on the mechanisms, purpose, and frequency of female ejaculation. What is it? Female ejaculation refers to the expulsion of fluid from a female's urethra during orgasm or sexual arousal. The urethra is the duct that carries urine from the bladder to the outside of the body. There are two different types of female ejaculate: Squirting fluid. This fluid is usually colorless and odorless, and it occurs in large quantities. Ejaculate fluid. This type more closely resembles male semen. It is typically thick and appears milky. Analysis has shown that the fluid contains prostatic acid phosphatase (PSA). PSA is an enzyme present in male semen that helps sperm motility. In addition, female ejaculate usually contains fructose, which is a form of sugar. Fructose is also generally present in male semen where it acts as an energy source for sperm. Experts believe that the PSA and fructose present in the fluid come from the Skene's glands. Other names for these glands include the paraurethral glands, Garter's duct, and female prostate. Skene's glands sit on the front, inside wall of the vagina near the G-spot. Researchers believe that stimulation causes these glands to produce PSA and fructose, which then move into the urethra. Is it real? For many years, scientists thought that females who ejaculated during sex were experiencing continence problems. Research has since disproved this idea and confirmed the existence of female ejaculation. A 2014 study found that the fluid accumulates in the bladder during arousal and leaves through the urethra during ejaculation. Seven women who reported experiencing female ejaculation during sex took part in the trial. First, the researchers used ultrasound exams to confirm that the participants' bladders were empty. The women then stimulated themselves until they ejaculated while the researchers continued to monitor them using ultrasounds. The study found that all the women started with an empty bladder, which began to fill during arousal. The post-ejaculation scans revealed that the participants' bladders were empty again. Is it normal and how common is it? Female ejaculation is perfectly normal, yet people do not discuss it very often. According to the International Society for Sexual Medicine, different estimates suggest that between 10 and 50 percent of women ejaculate during sex. Some experts believe that all women experience ejaculation, but that many do not notice. It is possible that they are not aware of it because the fluid can flow backward into the bladder rather than leaving the body. In an older study that involved 233 women, 14 percent of participants reported that they ejaculated with all or most orgasms, while 54 percent said that they had experienced it at least once. When the researchers compared urine samples from before and after orgasm, they found more PSA in the latter. They concluded that all females create ejaculate but do not always expel it. Instead, the ejaculate sometimes returns to the bladder, which then passes it during urination. What is known is that the experience of female ejaculation, including the feeling, triggers, and amount of ejaculate, varies considerably from person to person. Are there any health benefits? There is no evidence that female ejaculation has any health benefits. However, research has found sex itself to offer several benefits. During orgasm, the body releases pain-relieving hormones that can help with back and leg pain, headaches, and menstrual cramps. Immediately after climaxing, the body releases hormones that promote restful sleep. These hormones include prolactin and oxytocin. Other health benefits include: relieving stress boosting the immune system protecting against heart disease lowering blood pressure Connection to the menstrual cycle It is not clear whether or not there is a link between female ejaculation and the menstrual cycle. Some women say that they are more likely to ejaculate after ovulating and before menstruating, while others do not see a connection. More research is necessary to confirm or refute this association. Connection to pregnancy Some scientists believe that female ejaculate plays a role in pregnancy. They think this because the fluid contains PSA and fructose, which help sperm on their journey toward an unfertilized egg. Others dispute this theory, however. They argue that ejaculate usually contains urine, which can kill sperm. They also say that it is not easy for the fluid to travel from the urethra to the vagina, where it would need to be to play a role in pregnancy. Takeaway Female ejaculation is perfectly normal, and research suggests that it may be common despite people rarely discussing it. Scientists do not fully understand the biological purpose of female ejaculation or how it works. The experience of females who have ejaculated during sex varies considerably. |
|
#200
|
||||
|
||||
|
Re: Sexual Health News
What causes pelvic pain?
By Nicole Galan https://www.medicalnewstoday.com/articles/323960.php The pelvis is the area of the body below the abdomen or belly. There are many different organs and structures in the pelvis, including blood vessels, nerves, reproductive structures, bladder and urinary structures, and the bowel and rectum. There are many different causes of pain in the pelvis. In this article, we investigate possible causes of pelvic pain in men and women. We also look at the treatment options and when to see a doctor. Causes There are many causes of pelvic pain, including: 1. Constipation Constipation can cause pelvic pain, especially if it affects the lower colon. This type of pain tends to go away once a person has a bowel movement. 2. Other intestinal problems A variety of other intestinal conditions can cause pain in the lower abdomen or pelvis. These include: irritable bowel syndrome ulcerative colitis diverticulitis 3. Endometriosis Endometriosis is when tissue similar to the uterine lining grows outside of the uterus. This tissue can bleed during a person's menstrual cycle, as well as stick to other organs, causing pain and other symptoms. The location of the pain depends on where the tissue implants. While some people experience symptoms just during menstruation, others have pain at other times during their cycle. 4. Fibroids Fibroids are benign (non-cancerous) growths in the uterus. They can cause pain throughout the pelvis and lower back. Fibroids can also cause rectal or bladder pressure and the feeling of needing to go to the bathroom more often. 5. Pelvic inflammatory disease (PID) PID is an infection that occurs in the female reproductive structures. It is usually due to a sexually transmitted infection (STI). PID causes pelvic or low back pain, menstrual period changes, and unusual vaginal discharge. 6. Ovulation pain Ovulation pain or "mittelschmerz," is slight to moderate discomfort during the middle part of a menstrual cycle. Ovulation pain can last for a few minutes or up to a few days. The pain may feel like a cramp or be sharp and sudden. It is not indicative of any underlying problem. 7. Scar tissue or adhesions Previous infections or surgical procedures can cause the formation of scar tissue or adhesions in the pelvis. This type of scar tissue can cause chronic pelvic pain. 8. Adenomyosis Adenomyosis is when endometrial tissue grows deep into the uterine muscle. Women with this condition tend to have very heavy periods with severe pelvic pain. 9. Sexually transmitted infections (STIs) Most STIs do not cause any symptoms, but a few can cause pelvic cramping or pain. These include chlamydia and gonorrhea. Without treatment, some STIs can lead to PID, which can also cause pelvic pain. 10. Menstrual cramps Menstrual cramps occur in the lower part of the pelvis and tend to start just before a person's period and may continue for a few days. Particularly painful cramps could be a sign of an underlying condition, such as endometriosis or adenomyosis, so a person may wish to speak to a doctor about testing. 11. Ectopic pregnancy An ectopic pregnancy is a life-threatening event that requires immediate medical care. An ectopic pregnancy is when a fertilized egg implants into the pelvis or abdomen outside of the uterus. In most cases, an ectopic pregnancy occurs in the fallopian tubes, but it can happen anywhere in the abdomen or pelvis. Pain and cramping occur as it grows, pressing on nearby organs or nerves. 12. Pregnancy loss A pregnancy loss can also cause cramping or pelvic pain. Though some cramping in early pregnancy is normal as the fetus grows, people should report severe or long-lasting pain to a doctor. 13. Appendicitis The appendix is located in the lower abdomen and can cause pelvic or low back pain if it becomes inflamed and presses against the colon. 14. Hernia A hernia is an opening where the internal organs can pass through. If the hernia occurs in a muscle in the lower pelvis, it can lead to pelvic pain. Other symptoms may include a visible bulge at the location of the pain. 15. Muscle spasms in the pelvic floor The pelvis is made up of several muscles that support the bladder, reproductive structures, and bowel. Like other muscles, the pelvic floor muscles can spasm, causing pain and discomfort. 16. Prostate problems A man's prostate sits low in the pelvis. Inflammation or infection of the prostate can cause pelvic pain. A growth on the prostate, whether benign or cancerous, may also cause pelvic pain or discomfort. 17. Urinary tract infection (UTI) The typical symptoms of a UTI are burning pain during urination and more frequent urges to urinate. Some people also present with pelvic pain or cramping, especially for severe or long-lasting infections. 18. Interstitial cystitis Interstitial cystitis is a chronic bladder problem that causes pain in the lower pelvis, especially when delaying urination. People with interstitial cystitis usually experience frequent and urgent needs to go to the bathroom to urinate. 19. Kidney stones Stones formed in the kidney usually begin to make their way out of the body through the ureters and bladder, which can cause pain in the lower pelvis. This pain can be severe. 20. Ovarian mass A growth on the ovary can cause pelvic pain especially if it is pressing on the local nerves or nearby organs. Possible masses include an ovarian cyst, benign ovarian tumor, or ovarian cancer. Managing pelvic pain t is possible to manage the pain and discomfort once a person knows what is causing it. If a person is not sure of the cause or the pain is severe or does not improve, it is best to see a doctor. In many cases, simple home remedies can help relieve some of the pain. Home remedies to get relief include: taking over-the-counter pain relievers, such as ibuprofen placing a heating pad on the pelvis doing light and gentle exercise or stretching resting with the legs elevated, which promotes blood flow to the pelvis When to see a doctor While pelvic pain is a widespread problem, people should report it to a doctor, particularly if it does not respond to home remedies or is happening regularly. A person should seek medical help immediately if the pain is severe or they experience nausea or vomiting, fever, or loss of consciousness. It is best to contact a doctor with any questions or concerns about new or chronic pelvic pain. |
|
#201
|
||||
|
||||
|
Re: Sexual Health News
Never knew this about female ejaculation, quite interesting though
|
|
#202
|
||||
|
||||
|
Re: Sexual Health News
More than 1 million new curable sexually transmitted infections every day
6 June 2019 News release Geneva, Switzerland https://www.who.int/news-room/detail...ions-every-day Every day, there are more than 1 million new cases of curable sexually transmitted infections (STIs) among people aged 15-49 years, according to data released today by the World Health Organization. This amounts to more than 376 million new cases annually of four infections - chlamydia, gonorrhoea, trichomoniasis, and syphilis. “We’re seeing a concerning lack of progress in stopping the spread of sexually transmitted infections worldwide,” said Dr Peter Salama, Executive Director for Universal Health Coverage and the Life-Course at WHO. “This is a wake-up call for a concerted effort to ensure everyone, everywhere can access the services they need to prevent and treat these debilitating diseases.” Published online by the Bulletin of the World Health Organization, the research shows that among men and women aged 15–49 years, there were 127 million new cases of chlamydia in 2016, 87 million of gonorrhoea, 6.3 million of syphilis and 156 million of trichomoniasis. These STIs have a profound impact on the health of adults and children worldwide. If untreated, they can lead to serious and chronic health effects that include neurological and cardiovascular disease, infertility, ectopic pregnancy, stillbirths, and increased risk of HIV. They are also associated with significant levels of stigma and domestic violence. Syphilis alone caused an estimated 200 000 stillbirths and newborn deaths in 2016, making it one of the leading causes of baby loss globally. STIs remain a persistent and endemic health threat worldwide Since the last published data for 2012, there has been no substantive decline in either the rates of new or existing infections. On average, approximately 1 in 25 people globally have at least one of these STIs, according to the latest figures, with some experiencing multiple infections at the same time. STIs spread predominantly through unprotected sexual contact, including vaginal, anal and oral sex. Some—including chlamydia, gonorrhoea, and syphilis—can also be transmitted during pregnancy and childbirth, or, in the case of syphilis, through contact with infected blood or blood products, and injecting drug use. STIs are preventable through safe sexual practices, including correct and consistent condom use and sexual health education. Timely and affordable testing and treatment are crucial for reducing the burden of STIs globally, alongside efforts to encourage people who are sexually active to get screened for STIs. WHO further recommends that pregnant women should be systematically screened for syphilis as well as HIV. All bacterial STIs can be treated and cured with widely available medications. However, recent shortages in the global supply of benzathine penicillin has made it more difficult to treat syphilis. Rapidly increasing antimicrobial resistance to gonorrhoea treatments is also a growing health threat, and may lead eventually to the disease being impossible to treat. Expanding access to prevention, testing and treatment WHO generates estimates to assess the global burden of STIs, and to help countries and health partners respond. This includes research to strengthen prevention, improve quality of care, develop point-of-care diagnostics and new treatments, and generate investment in vaccine development. More data was available from women than men to generate these global estimates, and STI prevalence data remains sparse for men globally. WHO is seeking to improve national and global surveillance to ensure availability of reliable information on the extent of the STI burden worldwide. Published in the WHO Bulletin as an ‘online first’, the data provides the baseline for monitoring progress against the Global Health Sector Strategy on STIs, 2016–2021. The strategy, adopted by the World Health Assembly in May 2016, proposed rapid scale-up of evidence-based interventions and services to end STIs as a public health concern by 2030. read the study here Notes to editors The paper, Global and Regional Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2016, has been published in the WHO Online Bulletin as an ‘Online First’ pre-release. Online first articles have not yet been formatted and finalized with corrections from proofreaders so final text can change prior to print publication. About the four STIs Trichomoniasis (or “trich”) is the most common curable STI globally. It is caused by infection by a parasite during sexual intercourse. Chlamydia, syphilis and gonorrhoea are bacterial infections. Symptoms of an STI can include genital lesions, urethral or vaginal discharge, pain when urinating and, in women, bleeding between periods. However, most cases are asymptomatic, meaning people may not be aware they have an infection prior to testing. Chlamydia and gonorrhoea are major causes of pelvic inflammatory disease (PID) and infertility in women. In its later stages, syphilis can cause serious cardiovascular and neurological disease. All four diseases are associated with an increased risk of acquiring and transmitting HIV. Transmission of these diseases during pregnancy can lead to serious consequences for babies including stillbirth, neonatal death, low birth-weight and prematurity, sepsis, blindness, pneumonia, and congenital deformities. |
|
#203
|
||||
|
||||
|
Re: Sexual Health News
NUH cures patient of Hepatitis B by stopping medication in new trial
https://www.channelnewsasia.com/news...trial-11619346 SINGAPORE: Mr Arfan Awaloeddin was suffering from Hepatitis B for about 30 years, but in May this year, he was cured. All he had to do was stop taking his medication. The 49-year-old Indonesian is part of a National University Hospital (NUH) study that seeks to find out if Hepatitis B patients carrying a low amount of the markers of the viral infection have the best chances of being cured by stopping medication. Hepatitis B is a viral infection that affects the liver and was estimated to have been present in 180,000 people in Singapore in 2010, according to the latest figures available. Of the 23 people enrolled in the study that started in January, Mr Arfan is the first to be cured. The majority of them are men. Mr Arfan was diagnosed with the disease in 1992 or 1993 in his home country, and started getting treatment in Singapore in 1996. Speaking to the media at a sharing session at NUH on Wednesday (Jun 12), Mr Arfan said that he was initially scared to stop his medication. “I stopped medication on my own without asking my doctor in around 2000. I stopped for two to three months. I felt unwell, and after that I had to take medication again,” he said. But he was reassured when his doctor, senior consultant in the Division of Gastroenterology & Hepatology, Professor Lim Seng Gee, told him he would be monitored. Mr Arfan, who owns a hospital in Indonesia, said his father also suffered from Hepatitis B for 10 years before dying of liver cirrhosis in 2005. His three children, however, have been vaccinated against the disease. It is a new life now for Mr Arfan. “I feel good. I don’t have to spend money, I don’t have to take medication every morning. I feel free,” he said. He was spending about S$4,000 annually on his condition for consultation and medication, he said. Mr Arfan will be monitored monthly for the first year, in the three-year study. HOW STOPPING MEDICATION WORKS Typically, chronic Hepatitis B patients have to be on long-term medication, which could mean taking tablets daily. Prof Lim, the lead of the study, told the media said that when the medication is stopped, the virus will return. The patient’s immune system will then work to beat the virus. The virus becomes something new to the body although it has been carrying it because while the patient was on medication, the body did not recognise the virus as foreign, he explained. “When you stop treatment, suddenly, the body realises the virus is foreign, attacks it and clears it That’s what we think is the mechanism," said Prof Lim. When asked if that means they did not need therapy to start with, he said no. “We can’t say that, because originally, they were started on treatment because they needed it. But after 10 years, 20 years of treatment, is it time to stop? That really is the question,” he said. How the immune system is able to clear the virus when it was not able to before is something that researchers are still trying to find out, he said. Studies overseas have also shown that stopping medication cures Hepatitis B, but these did not focus on the amount of infection markers as a factor to find out which patients would benefit most from stopping medication, Prof Lim said. The trial in Singapore is the only one that is targeted at patients with low levels of infection markers. MINORITY WILL QUALIFY FOR STUDY In order to qualify for the study here, patients have to fulfil three criteria. Their infection markers have to be below the level of 100, they cannot have liver cirrhosis and they have to be on oral medication, said Prof Lim. Mr Arfan’s infection marker level was just two, much lower than the cutoff of 100, when he was enrolled. Typically, patients have levels that go into the thousands. While it is not known how many patients have such levels of markers, Prof Lim said it would be a minority who would qualify for it. The cutoff was based on other studies. Testing for the level of infection markers is relatively new, quite expensive and not in routine use, but patients can get tested for free as part of the study at NUH, Prof Lim said. “We do not know how common it is, so I would encourage patients to go and get it tested,” he said. The study, which will also start in Singapore General Hospital, Tan Tock Seng Hospital and Changi General Hospital, received S$1.5 million in funding from the National Medical Research Council. It will aim to enrol 150 patients. Of these, 50 will continue taking their tablets, so that the effectiveness of stopping medication can be compared against them. |
|
#204
|
||||
|
||||
|
Re: Sexual Health News
Can masturbation cause erectile dysfunction?
By Adrienne Stinson https://www.medicalnewstoday.com/articles/324068.php Some people believe that masturbation can cause erectile dysfunction, but this is a myth. Masturbation is a common and beneficial activity. While most men have trouble getting or keeping an erection at some point in their lives, frequent difficulties getting an erection is called erectile dysfunction (ED). Learn more about ED and masturbation, if watching porn affects sexual function, and when to see a doctor. Can masturbation cause ED? No, masturbation cannot cause ED — it is a myth. Masturbation is natural and does not affect the quality or frequency of erections. Research shows that masturbation is very common across all ages. Approximately 74 percent of males reported masturbating, compared to 48.1 percent of females. Masturbation even has health benefits. According to Planned Parenthood, masturbation can help release tension, reduce stress, and aid sleep. A person may not be able to get an erection soon after masturbating. This is called the male refractory period and is not the same as ED. A male refractory period is the recovery time before a man will be able to get an erection again after ejaculating. What does the research say? Universally, researchers are confident that masturbation does not cause ED. However, difficulty getting and keeping an erection either while masturbating or while having sex may be a sign of other conditions. Age is the most significant predictor of ED. Erectile dysfunction is common in men over 40 years old, with approximately 40 percent being affected to some degree. Rates of complete ED, or the inability to get an erection, increase from 5 percent in men aged 40 to about 15 percent at age 70. Other risk factors for ED include: diabetes being overweight heart disease lower urinary tract symptoms (bladder, prostate, or urethra issues) alcohol and cigarette use ED in younger men Although ED generally affects older men, a 2013 study found that as many as a quarter of men under 40 years old received a new ED diagnosis. In younger men, ED is more likely to be caused by psychological or emotional factors. Younger men also have higher levels of testosterone in their bodies and are less likely to have other risk factors for ED. Anxiety about sexual performance or erection quality can lead to further stress, sometimes creating a "vicious circle." Factors that can contribute to ED in younger men include: stress anxiety depression, post-traumatic stress disorder, bipolar disorder, or medications for these illnesses being overweight insomnia or lack of sleep urinary tract problems a spinal cord injury, multiple sclerosis, or spina bifida having a high-stress job relationship stress performance anxiety Porn and ED There is no evidence to suggest that watching porn causes ED. Internet porn usage rose at the same time that the rate of ED diagnoses increased in men under 40 years old. This led some researchers to believe that porn might affect male viewers' ability to get and maintain erections. While it is true that internet porn access and diagnoses of ED in younger men increased at about the same time and rate, this does not prove a link between the two. Until recently, there was little research into ED in young men, making numbers difficult to interpret. Also, due to stigmas and reluctance to speak to a doctor about sexual health, ED may be underreported in both younger and older men. It is also difficult to separate the psychological effect of watching porn from other psychological factors, such as performance anxiety. When to speak to a doctor ED is sometimes a sign of underlying conditions, such as heart disease or anxiety. Telling a doctor about ED can prevent potential problems that these conditions might cause, and also provide solutions to ED. For example, doctors may recommend that men with ED who are overweight lose some weight. This is because maintaining a healthy weight can increase testosterone levels, making it easier to get an erection. A doctor may also recommend stress-relief techniques or cognitive behavioral therapy for those dealing with ED due to emotional or psychological issues. Summary Masturbation does not cause ED, but many underlying health problems, including heart disease, urinary tract symptoms, alcohol use, depression, and anxiety, can. Research does not suggest that masturbation using internet porn could cause ED. Some people who watch porn may also experience performance anxiety, resulting in difficulties with erections, but performance anxiety is common without porn use. Anyone experiencing problems getting or maintaining an erection should speak to a doctor, as ED is often treatable. |
|
#205
|
||||
|
||||
|
Re: Sexual Health News
Orgasmic dysfunction: Everything you need to know
By Jenna Fletcher https://www.medicalnewstoday.com/articles/324112.php Orgasmic dysfunction is when a person has trouble reaching an orgasm despite sexual arousal and stimulation. In this article, learn about the causes and symptoms of orgasmic dysfunction and how to treat it. What is orgasmic dysfunction? Orgasmic dysfunction is the medical term for difficulty reaching an orgasm despite sexual arousal and stimulation. Orgasms are the intensely pleasurable feelings of release and involuntary pelvic floor contractions that occur at the height of sexual arousal. Orgasmic dysfunction is also known as anorgasmia. There are several different types of orgasmic dysfunction, including: Primary orgasmic dysfunction, when a person has never had an orgasm. Secondary orgasmic dysfunction, when a person has had an orgasm but then has difficulty experiencing one. General orgasmic dysfunction, when a person cannot reach orgasm in any situation despite adequate arousal and stimulation. Situational orgasmic dysfunction, when a person cannot orgasm in certain situations or with certain kinds of stimulation. This type of orgasmic dysfunction is the most common. Orgasmic dysfunction can affect both males and females but is more common in females. Researchers estimate that female orgasmic disorder, which is recurrent orgasmic dysfunction, may affect between 11 to 41 percent of women. The North American Menopause Society report that 5 percent of all women have difficulty achieving orgasm. Research from 2018 found that 18.4 percent of women could reach an orgasm through intercourse alone. However, the same study indicated another 36.6 percent of women needed clitoral stimulation to reach orgasm during intercourse. In men, experts often categorize orgasmic dysfunction and delayed ejaculation together. Available studies suggest that delayed ejaculation is very uncommon in men, with one 2010 overview noting that it was rarely prevalent in more than 3 percent of men, although other estimates have the figure between 5 and 10 percent. Orgasmic dysfunction can affect the quality of people's relationships, as well as a person's self-esteem and mental health. Symptoms Orgasmic dysfunction is when someone has difficulty or the inability to reach an orgasm. For some people, reaching a climax can take longer than normal or be unsatisfying. The way an orgasm feels or how long it takes to have an orgasm can vary widely. When someone has orgasmic dysfunction, climax can take a long time to reach, be unsatisfying, or be unattainable. Causes Scientists are not sure what causes orgasmic dysfunction, but believe the following factors may contribute to the problem: relationship issues certain medical conditions, such as diabetes a history of gynecological surgeries some medications, including antidepressants a history of sexual abuse religious and cultural beliefs about sex and sexuality depression anxiety stress low self-esteem Also, women over 45 years of age are more likely to have trouble orgasming than women under this age. This may be due to menopause-related hormonal shifts and vaginal changes. Men are more likely to have trouble orgasming following a radical prostatectomy. They are also more likely to experience delayed ejaculation as they get older, as the ejaculatory function tends to reduce with age. Once someone experiences difficulty reaching an orgasm, they may experience increased stress in sexual situations. Stress and anxiety during sex can make it even more difficult to reach an orgasm. Diagnosis Before diagnosing orgasmic dysfunction, a doctor will likely ask about a person's symptoms and how long they have existed. The doctor will also note any factors that could contribute to orgasmic dysfunction, such as underlying health conditions or the medications a person is taking. A doctor may do a physical examination as well. In some cases, they may refer a person to a sexual medicine specialist or a gynecologist. Treatment Treatment for orgasmic dysfunction varies, depending on the underlying cause. A doctor may recommend treating any other conditions or adjusting any medications that may contribute to sexual health problems. In many cases, a doctor may recommend a person who has orgasmic dysfunction try sex therapy or couples counseling. A certified sex therapist can offer psychotherapy that focuses on concerns related to sexual function, feelings, or dysfunctions. Sex therapy can be done on an individual basis or with a partner. Couples counseling focuses on relationship issues that may be affecting an individual's sexual function and their ability to orgasm. In some cases, a doctor or therapist may suggest a person try other forms of sexual stimulation to reach orgasm, such as masturbation or increased clitoral stimulation during intercourse. For others, they may recommend over-the-counter oils and warming lotions. Hormone therapy may be effective for some females, particularly if the inability to orgasm coincided with the start of menopause. In these cases, a doctor may suggest the woman tries an estrogen cream, patch, or pill. The estrogen may alleviate some menopause symptoms and improve sexual response. While situational orgasmic dysfunction is not uncommon, people should speak with their doctor if they have any concerns about their ability to orgasm. Summary Orgasmic dysfunction is the medical name for the inability to reach orgasm. Some people may experience orgasmic dysfunction when it takes too long to reach orgasm or when their orgasm does not feel satisfying. Many factors can contribute to orgasmic dysfunction. To remedy orgasmic dysfunction, a person can speak to a doctor, a certified sex therapist, and other medical professionals to find the cause. People can take steps to treat orgasmic dysfunction and improve their sexual health once they know the cause. |
|
#206
|
||||
|
||||
|
Re: Sexual Health News
How to tell if a penis rash is from HIV
By Jenna Fletcher https://www.medicalnewstoday.com/articles/324289.php Similarly to other viral infections, an early symptom of HIV is a rash that can appear anywhere on the body, including the penis. When HIV causes a rash, it appears as a flat red patch with small red bumps. Itchiness is the primary symptom of an HIV rash. HIV rashes typically appear on the upper areas of the body, but sometimes, a rash can develop on the penis. In this article, we examine the signs and how to identify an HIV rash when it appears on the penis. HIV rash symptoms A rash is one of the earliest symptoms that a person might experience after contracting HIV. According to the U.S. Department of Health and Human Services, an HIV rash typically appears during the acute stage of infection, which can last 2 to 4 weeks after contracting HIV. The rash can last for 1 to 2 weeks as the body tries to fight the infection. The rash often appears as a red area of skin with tiny bumps. It is often itchy and may be painful. The rash typically occurs alongside other flu-like symptoms including: fever a sore throat swollen glands fatigue joint and muscle pain Similar to the rash itself, the other symptoms should clear up within about 2 weeks. There are several potential causes of HIV rash including: the HIV infection itself HIV medication side effects other infections other medications It is essential to know what an HIV rash looks like because this means a person can seek medical assistance sooner. When an HIV rash appears, it can spread over large areas of the body, including the penis. The rash typically consists of small round, red bumps that may be flat or raised. Sometimes, the bumps have a crusty, white appearance or they may resemble small scabs. Other symptoms Without treatment, HIV will continue to damage the immune system. A person may not experience any other symptoms from the virus during this time. This may mean they do not develop a rash. Some people may develop ulcers that appear in their mouth, the esophagus, in or around the anus, or on the penis. Sometimes, lymph nodes, which are under a person's arm or in their neck, swell up. The swelling could last for much longer than the rash or flu-like symptoms. As HIV progresses, sometimes over many years, it can compromise a person's immune system. As a result, some people may experience: recurrent infections that last for long periods weight loss night sweats chronic diarrhea life-threatening infections skin issues When to see a doctor Anyone who develops a rash on their penis may want to talk to their doctor. A person should seek medical attention if they experience flu-like symptoms alongside the rash and they think they may have contracted or had exposure to HIV. However, there is a range of other potential reasons for a rash on the penis that are less serious than HIV. These include: balanitis, which is a swelling of the penis tip often due to poor hygiene a yeast infection or another fungal infection scabies, which is a contagious itchy rash due to mites contact dermatitis or allergic reaction on the skin A person may also develop a rash from sexually transmitted infections (STIs), including: herpes syphilis chancroid, which is an infection that causes sores on the genitals pubic lice If a doctor suspects that a person has HIV, they will order an HIV test. Though there are a few potential options, the most accurate is a blood test. Results come back either negative if no infection is present or positive if there is evidence of an infection. Even if the test comes back negative, a person who believes they may have had exposure to HIV should receive testing frequently. Early detection is key to treatment. The earlier treatment begins, the better a person's outlook. With successful treatment, many people with HIV have a normal life expectancy. Typically, doctors prescribe creams or ointments to treat a rash on the penis, but which one will depend on the precise cause of the rash. Takeaway HIV can cause a rash on the penis. The rash may occur alongside flu-like symptoms, such as a fever, muscle aches, and swollen glands. If these symptoms appear together, seek medical attention. Early treatment of HIV is key to successfully managing the disease. |
|
#207
|
||||
|
||||
|
Re: Sexual Health News
What to know about friction burns on the penis
By Jenna Fletcher https://www.medicalnewstoday.com/articles/325533.php Friction burns can appear on the penis as a result of vigorous rubbing, which may occur during sexual activity or when a person wears very tight fitting clothing. A friction burn happens when contact with another object causes the skin on a body part to rub off. Friction burns can be very painful, especially on such a sensitive area of the body. According to the authors of a review paper, it is difficult to determine the prevalence of friction burns on the penis because ethical and psychological reasons often prevent people from reporting injuries to this part of the body. Read on to learn more about friction burns on the penis and how to treat and prevent them. Symptoms A friction burn on the penis will have similar symptoms to those of friction burns on other parts of the body. It is important to recognize the symptoms of a friction burn on the penis so that a person can distinguish between this injury and other more serious issues, such as sexually transmitted infections (STIs). The symptoms of a friction burn on the penis include: red, swollen skin on the penis an area of skin on the penis that may look like a cross between a scrape and heat burn pain in the affected area These symptoms can also occur as a result of other more serious issues. For example, the following conditions can also cause penile pain and redness: gonorrhea chlamydia herpes syphilis a yeast infection in the penis balanitis The other symptoms of a more serious health issue may include: penile discharge that can be yellow, green, or watery itching inside the penis painful or swollen testicles sores on the penis or testicles pain or burning with urination A person with any of the above symptoms should see their doctor immediately.  Causes Intense rubbing generally causes friction burns. Most friction burns that doctors see in a healthcare setting are due to a road accident. However, there are other possible causes of a friction burn on the penis, including: vigorous masturbation intense sexual intercourse wearing tight fitting clothing that rubs the penis during exercise drying the penis too vigorously with a coarse towel Friction burns from masturbation and sexual intercourse may be more likely to occur if a person does not use lubrication. Treatment The best way to treat a friction burn is to give the area time to heal without doing the activity that caused the burn to occur. Most minor friction burns should go away on their own in time. It is possible to treat most friction burns on the penis at home. While a person is waiting for a penile friction burn to heal, they should do the following to help make themselves more comfortable and prevent further irritation to the penis: wear loose fitting, breathable clothing in soft fabrics avoid the penis coming into contact with coarse materials apply moisturizer, aloe, or petroleum jelly to the affected area to protect the skin while it heals avoid sex, masturbation, and similar activities until the area heals If the affected skin starts to ooze or drain pus, a person should make an appointment with their doctor. Pus is a sign of infection, and a topical antibiotic may be necessary to help the affected area heal. Prevention During sexual activity with a partner, using a lubricated condom can help prevent friction burns. Aside from preventing penile friction burns, condoms can also prevent unplanned pregnancy and help keep both partners healthy by reducing the risk of STIs. Additionally, a person can ask their partner to be gentler or use lubrication during sexual activity. One of the best ways to prevent friction burns on the penis when masturbating is for the person to be more gentle with themselves. Using a water-based lubricant can also help prevent friction burns. Many forms of water-based lubricant are available to purchase online. People can take other steps to help reduce skin irritation that can cause friction burns, including: Proper hygiene. Keeping the penis clean by washing it daily with gentle soap and warm water can help prevent irritation. It helps to wash underneath the foreskin, the base of the penis, and the testicles every day. Gentle and complete drying. After having a shower, be sure to dry the penis thoroughly but gently. Instead of rubbing to dry the penis, pat it dry with a soft towel. Wear proper clothing. Avoiding clothes that are too tight and not breathable can help prevent irritation, especially when exercising. People should also be aware of how other health issues can affect the penis. For example, if a person has diabetes that they find difficult to manage, they may be more at risk of yeast infections that can cause penile irritation. Untreated STIs can also irritate this part of the body. Summary Friction burns on the penis can be painful. A person can treat most friction burns at home unless the burn becomes infected. If this occurs, they should see a doctor. The best treatments for friction burns are time and rest from the activity that caused the burn. A person can help prevent friction burns on the penis by avoiding vigorous sexual activity and not wearing tight fitting clothing, especially when exercising. Good hygiene can also help keep a penis healthy. |
|
#208
|
||||
|
||||
|
Re: Sexual Health News
What Causes Red Spots on the Penis and How Are They Treated?
https://www.healthline.com/health/me...-spot-on-penis Should I be concerned? If red spots have formed on your penis, it’s important to remember that they aren’t always a sign of something serious. In some cases, red spots may result from poor hygiene or a minor irritation. These spots typically disappear in a day or two. Red spots that develop as a result of something more serious, such as a sexually transmitted infection (STI), typically last longer and are accompanied by other symptoms. Read on to learn what symptoms to watch for, how each condition might be treated, and when to see your doctor. What do the red bumps look like? If you’re looking for a quick diagnosis, you can use the following chart to assess your spot symptoms. This chart is only assessing the appearance, feel, location, and number of spots — it isn’t accounting for any other symptoms that you may be experiencing. If you’re leaning toward one or two different conditions based on spot symptoms, read more about them below to assess any other symptoms, learn treatment options, and see whether you should visit your doctor.  Genital herpes Genital herpes is an STI that can cause red spots on your penis, as well as your: scrotum pubic area at the base of the penis thighs buttocks mouth (if it’s passed through oral sex) Genital herpes results from the herpes simplex virus (HSV-2 or, less frequently, HSV-1). This virus enters your body during unprotected sex with someone who carries the virus. Other symptoms include: pain or discomfort itchiness ulcers that bleed or drain when blisters pop scarring or scab development when ulcers get better Options for treatment See your doctor if you think you have genital herpes. It isn’t curable, but your doctor may prescribe antiviral medications, such as valacyclovir (Valtrex) or acyclovir (Zovirax), to ease your symptoms and prevent it from spreading to your sexual partners. Syphilis Syphilis is an STI caused by Treponema pallidum. This bacterium is spread through unprotected sex with someone who’s infected. The first symptom is often a circular, red, painless sore on your penis and genital area. If left untreated, it can spread and advance to other parts of your body. As the infection progresses, you may experience: rash on other parts of your body, such as your torso fever of 101°F (38.3°C) or higher lymph node swelling headaches paralysis Options for treatment Seek immediate medical attention if you think you have syphilis. The longer it’s untreated, the more severe and irreversible your symptoms may become. In its early stages, syphilis can be successfully cured with injected or oral antibiotics, such as: benzathine penicillin ceftriaxone (Rocephin) doxycycline (Oracea) You shouldn’t engage in sexual activity until a follow-up blood test shows that the infection has cleared. Scabies Scabies happens when mites burrow into your skin to live, eat skin cells, and lay eggs. These mites are spread through close contact — usually sexual activity — with someone who already has them. The most notable symptoms are itching and irritation where the mite dug into your skin. Other symptoms include: dry, scaly skin blisters white-colored lines in the skin where mites have burrowed Options for treatment See your doctor if you think you have scabies. They’ll likely prescribe a topical cream, such as permethrin (Elimite) or crotamiton (Eurax), to treat and clear the infestation. You should follow their instructions for application closely. Molluscum contagiosum Molluscum contagiosum is a skin infection caused by a poxvirus. It’s spread through skin-to-skin contact or by sharing towels, clothes, bedding, or other materials with someone who’s infected. It typically results in red, itchy bumps on your penis and other affected areas. Scratching can irritate the bumps and cause the infection to spread to other areas of the body. Options for treatment Molluscum contagiosum often goes away on its own, so you don’t need to seek treatment right away. To relieve symptoms, your doctor may recommend one or more of the following: topical therapies to dissolve bumps cryosurgery to freeze and remove bumps curettage to cut bumps out from the skin laser surgery to destroy bumps Balanitis Balanitis is irritation of the head (glans) of your penis. It’s usually caused by poor hygiene or an infection. You’re more likely to develop balanitis if you’re uncircumcised. Red spots, swelling, and itching are common symptoms. Other symptoms include: pain while urinating fluid buildup under the foreskin inability to pull back your foreskin (phimosis) Options for treatment In some cases, balanitis can be resolved by practicing good hygiene. You should keep your penis clean by regularly washing under your foreskin. Use natural, unscented soaps and pat your penis and the area under your foreskin dry. If your symptoms linger or don’t improve after a couple of days, see your doctor. You may be experiencing an infection. Your doctor may prescribe: steroid creams, such as hydrocortisone antifungal creams, such as clotrimazole (Lotrimin) antibiotics, such as metronidazole (Flagyl) Contact dermatitis Contact dermatitis is a skin reaction from touching something you’re allergic to. Immediate symptoms include: swelling itching dry, scaly skin pus-filled blisters that burst and ooze If the bumps start oozing and become infected, you may also experience symptoms like fatigue and fever. Options for treatment Contact dermatitis usually goes away on its own. You may find it helpful to: apply a cold compress sit in a warm oatmeal bath take over-the-counter antihistamines, such as diphenhydramine (Benadryl) Shop for antihistamines. You should see your doctor if: your blisters pop you have a fever the rash spreads beyond your penis Your doctor may recommend prescription-strength antihistamines or other therapies to help ease your symptoms. Yeast infection A yeast infection, or thrush, is an infection caused by the Candida fungus. It’s usually a result of poor hygiene or sex with someone who’s infected. The most common symptoms are red spots or irritation in the genital area. The area may also itch. Other symptoms include: smelliness trouble retracting your foreskin (phimosis) a white, chunky substance at the tip of your penis or under your foreskin Options for treatment A yeast infection can go away on its own with improved hygiene and looser clothing. If your symptoms are severe or last for more than a few days, see your doctor. They may prescribe antifungal creams or oral medication, such as clotrimazole, to help ease your symptoms. Jock itch Jock itch, or tinea cruris, is a genital infection caused by dermatophyte fungi. It usually happens when you sweat a lot or don’t wash your genital area well enough. The most common symptoms are red spots or a rash in your genital area. Your skin may also appear dry, scaly, or flaky. Options for treatment Improved hygiene can help relieve symptoms. If your symptoms are severe or last for more than a few days, see your doctor. They may prescribe an antifungal cream or ointment, such as clotrimazole. Genital eczema Atopic dermatitis (eczema) is a skin condition that can cause irritation on your penis. It’s usually a result of both genetic and environmental factors like stress, smoking, and allergens. The most common symptoms are red, irritated spots or a rash in your genital area. Other symptoms include: dry, scaly skin constant itching pus-filled blisters that crust over Options for treatment If you suspect your symptoms are the result of an eczema flare, see your doctor. They may be able to recommend new or different therapies to help ease your symptoms and prevent flare-ups. This includes: antibiotic creams, such as mupirocin (Centany) calcineurin inhibitors, such as pimecrolimus (Elidel) topical corticosteroids, such as hydrocortisone injectable biologics, such as dupilumab (Dupixent) In the meantime, you may find it helpful to: apply a cold compress apply lotion, moisturizer, or aloe vera Shop for lotion, moisturizer, and aloe vera now. Genital psoriasis Psoriasis happens when skin cells grow too quickly and cause irritation. It's likely caused by an immune system condition in which your white blood cells mistakenly attack skin cells. The most common symptoms are red, itchy bumps or a rash in your genital area. Other symptoms can include: dry or sore skin that bleeds joints feeling stiff or swollen thick or ridged fingernails or toenails Options for treatment If you suspect your symptoms are the result of a psoriasis flare, see your doctor. They may be able to recommend new or different therapies to help ease your symptoms and prevent flare-ups. This includes: topical corticosteroids, such as hydrocortisone phototherapy, which exposes the skin to concentrated UV light retinoids, such as acitretin (Soriatane) biologics, such as adalimumab (Humira) Shop for hydrocortisone. In the meantime, you may find it helpful to: apply lotion, moisturizer, or aloe vera take baths every day limit or avoid alcohol and tobacco intake When to see your doctor Regardless of the suspected cause, you should see your doctor if: the spots become unbearably painful or itchy the spots show signs of infection you notice STI symptoms like fatigue and fever Your doctor can assess your symptoms and make a diagnosis, if needed. They can also offer information on how to ease your symptoms at home or prescribe any necessary medication. |
|
#209
|
||||
|
||||
|
Re: Sexual Health News
What causes cloudy urine?
By Jon Johnson https://www.medicalnewstoday.com/articles/324443.php Cloudy urine can be unsettling, especially when a person does not know the cause. Sometimes it can signal an issue with the urinary tract, such as dehydration or a urinary tract infection, or it may point to kidney problems. Each underlying cause of cloudy urine has additional symptoms, which can help a doctor make a diagnosis. In this article, learn about the possible causes of cloudy urine, as well as how to treat them. Causes Causes of cloudy urine can include: 1. Dehydration Cloudy urine, especially if it is dark, could indicate that a person is not consuming enough liquids. Very young or very old people have a higher risk of dehydration. Also, anyone fighting off an illness that causes diarrhea, vomiting, or a fever will need to drink more fluids. Those who do strenuous exercise or physical labor during hot days may also have a higher risk for dehydration if they are not drinking enough water. Dehydration can cause cloudy urine in some people, as well as other symptoms, including: dark yellow or orange urine fatigue confusion or difficulty concentrating dizziness dry mouth and a feeling of intense thirst dry eyes less frequent urination Severe dehydration can cause more severe symptoms, including disorientation, a loss of consciousness, or bloody or black stools. Seek emergency medical care for severe dehydration. 2. Urinary tract infection (UTI) A UTI is another more common cause of cloudy or milky urine. If the urine smells particularly foul, a person may have an infection. The cloudy look typically comes from discharge of either pus or blood into the urinary tract. It could also be a buildup of white blood cells as the body tries to eliminate invading bacteria. UTIs can happen in anyone but are far more common in females, according to the United States Office on Women's Health. Along with cloudy urine, a UTI can cause other symptoms, such as: a constant need to urinate trouble urinating large amounts or emptying the bladder burning pain while urinating foul-smelling urine pain in the pelvis, lower abdomen, or lower back Anyone who experiences these symptoms should see a doctor for diagnosis and treatment. Treating a UTI early can help relieve discomfort and prevent complications. 3. Kidney infection Many kidney infections start as UTIs, which then spread due to lack of effective treatment and get worse over time. Kidney infections cause similar symptoms to UTIs and may also cause additional symptoms, such as: a fever chills cramps fatigue nausea and vomiting pain in the back, side, or groin dark, bloody, or foul-smelling urine Kidney infections require immediate medical treatment. Without prompt treatment, this type of infection may lead to permanent kidney damage. 4. Sexually transmitted infection (STI) According to the Office on Women's Health, about 20 million people in the U.S. get an STI every year. Some common STIs, such as gonorrhea and chlamydia, may cause cloudy urine. Gonorrhea and chlamydia prompt the immune system to fight back and produce white blood cells, which may mix with the urine and give it a cloudy appearance. These STIs may also cause unusual discharge from the vagina or penis. Other signs of an STI include: itching of the genitals or pelvis unexplained pain in the genitals pain during or after sex pain or burning during urination or ejaculation rashes, blisters, or other sores on the genitals Regular testing for STIs can help a person receive an early diagnosis and get treatment. Using protection during sexual activity may also help prevent the spread of STIs. 5. Vulvovaginitis Vulvovaginitis is inflammation in the vulva and vagina, and it can lead to cloudy urine. Bacterial infections are the most common cause of vulvovaginitis, though the infection can also result from viruses or fungi. In some cases, the body may react to ingredients in soaps, detergents, fabric softeners, or other products. These reactions can cause inflammation in the vulva and vagina without an infection being present. Other signs of vulvovaginitis include: itchiness around the vulva foul-smelling vaginal discharge thin, pale, watery discharge discolored discharge that resembles cottage cheese a fishy odor that gets worse after sex painful urination A doctor will want to determine whether the infection is bacterial, fungal, or viral before moving forward with treatment. 6. Prostatitis An inflamed prostate, or prostatitis, may also be the cause of cloudy urine. The U.S. Department of Health and Human Services state that prostatitis affects between 10 and 15 percent of the males in the United States. It typically appears due to an infection in the prostate. Other symptoms of prostatitis include: painful ejaculation pain or burning sensations while urinating a frequent need to urinate blood in the urine abdominal pain pain in the lower pelvis, genitals, or perineum 7. Kidney stones Kidney stones can also cause cloudy urine. They develop from the buildup of certain minerals in the body. Small stones may pass without incident, but larger stones can block the urinary tract and cause an infection, which could lead to pus in the urine, giving it a cloudy appearance. A common symptom of kidney stones is severe pain below the ribs, generally near the side or lower back. The pain may also occur in the groin and radiate to the lower abdomen or lower back. Other symptoms of kidney stones include: fever chills pain while urinating brown, red, or pink streaks in the urine foul-smelling urine Some kidney stones do not require treatment. However, anyone who thinks that they may have kidney stones should see a doctor for a diagnosis. 8. Diet In some cases, a person's diet can cause their urine to be cloudy. Anyone who consumes high amounts of vitamin D or phosphorus may notice cloudy urine as their kidneys filter the excess phosphorus out of their body. The U.S. National Kidney Foundation state that protein-rich foods such as meat, beans, and dairy products may be higher in phosphorus. 9. Diabetes or kidney damage from diabetes Sometimes diabetes or diabetic kidney disease is the underlying cause of cloudy urine. The body may be trying to remove excess sugars that it cannot process by sending them through the urine. Other signs of diabetes may include issues such as: prolonged thirst, even after drinking fatigue weight loss a frequent need to urinate frequent infections difficulty healing from simple wounds Untreated, the issues from diabetes may ultimately lead to kidney failure. Anyone who has diabetes or experiences these symptoms should talk to their doctor, who can check for signs of kidney damage. Diagnosis If cloudy urine accompanies other symptoms, see a doctor for a diagnosis. The doctor may ask for a urine sample, which they will test for infections. They may also test for common STIs. Depending on a person's symptoms, the doctor may also recommend blood tests to check for signs of kidney damage. Treatment Treatment for cloudy urine will depend on the underlying cause. Typical treatments for each issue include: Dehydration: Treating dehydration may be as simple as drinking more fluids and eating foods that are rich in liquids. Severe dehydration may require hospitalization, however. UTIs: Most UTIs respond well to a round of antibiotics. In more severe cases, the person may need to receive these drugs intravenously, then orally. STIs: Treatment will depend on the type of STI. Infections such as gonorrhea and syphilis generally respond well to antibiotics. Kidney stones: Many stones pass naturally. A doctor may prescribe pain medication if the stones are very painful. For larger stones, the doctor may prescribe medications or shock wave therapy to break them into passable pieces. Very large stones may require surgery. Vulvovaginitis: The doctor may recommend antibiotic, antifungal, or antiviral medication to treat vulvovaginitis and clear up symptoms. Prostatitis: Prostatitis may get better without treatment. If bacteria are causing the infection, antibiotics may help treat symptoms. For chronic cases, doctors may recommend medications to manage symptoms. Diabetes: Kidney problems arising from diabetes may require frequent urine tests to check for damage in the kidney. A person will also require treatment for the underlying diabetes. Summary Cloudy urine can result from a variety of common conditions, such as UTIs and mild dehydration. In cases that occur with other symptoms, early diagnosis and treatment are key to avoid complications. Take note of any other symptoms that appear and share them with the doctor. This may determine the diagnosis and appropriate treatment. By working with a doctor and following their instructions, most people can clear up the underlying cause of cloudy urine. |
|
#210
|
||||
|
||||
|
Re: Sexual Health News
5 menstruation myths you must leave behind
By Maria Cohut https://www.medicalnewstoday.com/articles/324403.php Approximately half of the world's population experiences, will experience, or has experienced menstruation, and yet myths about this biological process still abound. In this Spotlight feature, we debunk some of the most widespread menstruation misconceptions. As of 2017, the world's population numbers 7.53 billion people, of which 3.73 billion are born with female genitalia. Virtually all of them do, have, or will go through menstruation (period), the part of the menstrual cycle in which the uterus sheds mucosal tissue alongside blood through the vagina. Periods can last between 3 and 7 days and usually occur every 28 days, though menstrual cycle lengths can vary. Although this biological process affects about half of the world's population, many myths and misconceptions about it persist. Cultures around the world still vilify menstruation, and consider period blood "dirty" and "impure," and menstruation itself as a taboo topic. For instance, although this practice is now mostly illegal, some communities — as a series of recent tragedies in Nepal suggest — still have the so-called menstruation huts, in which women on their period spend the days in which they bleed in complete isolation. Though this is an extreme example, there are many smaller myths and misconceptions related to menstruation that remain in circulation across the globe. Read this Spotlight feature to find out what some of the most popular misconceptions are, and why they are untrue. 1. Sex on your period Some of the most widespread myths regarding menstruation gravitate around sex while on your period, with the top contender likely being that you cannot get pregnant while menstruating. However, this idea is entirely false. While it is true that, in many individuals, menstruation is the period when they are least fertile, it really depends on the length of their monthly cycles. Peak fertility occurs during the ovulation stage — which usually kicks in approximately 12 to 16 days before the start of the next period — when the ovaries produce and release fresh ovules (eggs). And while most menstrual cycles last about 28 days, some cycles can be as short as 21 days, which also impacts when ovulation takes place. Moreover, sperm can live inside the genital tract for up to 5 days or, according to some sources, even 7 days. Thus, having unprotected vaginal sex during your period could mean that the sperm gets to linger for just long enough to coincide with ovulation and fertilize an egg, resulting in pregnancy. Moreover, if you have sex during menstruation without using a condom, the risk of getting a sexually transmitted infection (STI) — including HIV — or a yeast infection increases, due to the hormonal changes that occur at this time. Vaginal-penile sex during a period can also, in some cases, cause inflammation of the penis head — a type of infection called "balanitis." Still, as long as you take all necessary precautions to avoid an unwanted pregnancy and the transmission of STIs, there is no reason not enjoy sex while on your period — to the contrary, in fact, as sex can help relieve cramps and improve your mood. 2. Unsafe to keep skipping your period? Another widespread misconception is that it is unsafe to use birth control pills to enable you to skip your period for a prolonged period. However, recent guidelines from the National Women's Health Network indicate that it is just fine to suppress menstruation through birth control pills, and most gynecologists agree that this approach is typically safe. Some people even argue that, outside of their role in reproduction, periods are unnecessary, and can be more trouble than they are worth. For instance, James Segars, from the department of gynecology and obstetrics at Johns Hopkins University in Baltimore, MD, told The Atlantic that, "Having a monthly period is reassuring, but it is certainly not necessary." "And with these long-term, reversible contraceptives, the failure rate is really, really low so women can benefit a lot from them." James Segars For many individuals, menstruation symptoms can be severe and interfere with their normal functioning and quality of life. They may experience heavy bleeding, disabling pain, and other unpleasant symptoms, such as migraines and nausea. Those with dysmenorrhea (painful periods) or certain conditions that cause troublesome symptoms, such as endometriosis, may decide, in agreement with their doctors, that skipping several periods, or skipping menstruation continuously, is the best option for their health and productivity. 3. Shouldn't have a bath Some think that having a bath or even taking a shower during your period is unsafe. This is either because hot water stimulates bleeding, or because the water stops you from bleeding, which can have ill effects. While hot water can help stimulate blood flow, this can actually help relieve menstrual cramps and ease muscular tension. Bleeding does not stop following full immersion in water. However, the pressure from the water may temporarily prevent the blood from flowing out of the vagina. There is no reason not to have a bath or shower during your period. Most likely, relaxing in a bubble bath and feeling cleaner as a result of it will improve your mood and help you cope with menstruation symptoms a little better. Furthermore, it is better and healthier to use water and mild, unfragranced soap to clean the vulva than wipes or other products. This is because many intimate care products can disrupt the delicate bacterial balance in the genital area, making it easier for infections to take hold. A study that Medical News Today reported on last year found a "strong correlation" between the use of intimate care products, such as gel sanitizers and vaginal cleansers, and a heightened risk of infection. Plus, having a hot bath could bring a host of other health benefits. One study covered on MNT last year suggested that baths may reduce inflammation and improve blood sugar. 4. Syncing periods One pervasive question surrounding periods is whether can they actually sync. For example, if two or more women spend enough time together, perhaps as roommates, will they have periods at the same time? One person, speaking to MNT, said that she was even taught about period synchrony in school, and was still wondering whether the notion was accurate. She told us: "I heard about period syncing a long time ago when I studied in an all-girls' school. Then, when I started living with [my two female roommates], I noticed we often had periods around the same time. [Another friend] says that this is due to an alpha-female releasing hormones that affect the period cycles of other women around her." So is any of this true? After all, many of us are likely to have experienced "period syncing" at some point, in a school, work, or home-sharing environment. The notion of "period synchrony" first appeared as a scientific idea in a 1971 Nature article. This article argued that women who lived in close quarters — roommates in a college dorm — or who were close friends, experienced increased menstruation synchrony. The study's authors believed that this probably happened because the women who lived so closely together "exchanged" pheromones over time, which eventually led to this phenomenon. However, later studies cast doubts on the methodology researchers used for the 1971 research. The later studies highlighted numerous shortcomings and modifying factors that the original researchers had not accounted for. They also noted a "lack of empirical evidence for synchrony in the foregoing studies of both Western and non-Western populations." Moreover, studies that followed were never able to replicate the findings of the initial research. convincingly. Research published more recently did not find that college roommates experienced menstrual synchrony. Investigators have since become more inclined to believe that the notion is nothing but an enduring myth, with any synchrony being purely coincidental. Alexandra Alvergne, who is an associate professor in biocultural anthropology at the University of Oxford in the United Kingdom, told the BBC that, "As humans, we always like exciting stories. We want to explain what we observe by something that is meaningful. And the idea that what we observe is due to chance or randomness is just not as interesting." 5. Tampon myths Finally, some of the most persistent misconceptions refer to the use of tampons to absorb period blood. Because a person has to insert a tampon in the vagina, some people may worry that this may cause some damage. One primary worry is that inserting a tampon can break the hymen, which, as popular misconception has it, is a "mark of virginity." In reality, the hymen is a stretchy membrane that lines the opening of the vagina and does not ordinarily cover the vaginal opening. If this were the case, the hymen would block menstrual blood and other types of discharge from leaving the body. This would be dangerous, requiring surgical intervention to correct. Because the hymen is stretchy, inserting an object as small as a tampon will not cause any tears. And since, during menstruation, the blood lubricates the vagina, inserting a tampon should not be uncomfortable, if done correctly. If still uncomfortable, try using a lubricant to help slide the tampon in. A person should always change tampons regularly, as recommended, about every 4-8 hours. It is essential that a person does this otherwise the accumulated blood, tissue, and bacteria could cause toxic shock syndrome. A second myth that many first-time tampon users have encountered is that a tampon could get lost inside the vagina. This is just not true because there is nowhere for the tampon to go. The cervix is at the top of the vagina, and its opening is much too small for a tampon to penetrate. Moreover, vaginas are only about 3.77 inches (9.6 centimeters) deep, on average, and tampons come with strings that aid removal. So, if the tampon does happen to ride up somewhat, you can always easily search for the string and pull the tampon out carefully. Should you ever encounter a piece of information that you are unsure about, or which you find alarming, speak to a nurse or a doctor, who will be able to fact check it for you. Myths and misconceptions have no place in healthcare. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |