 |
|
#181
|
||||
|
||||
|
Re: Sexual Health News
Sex after a C-section: Everything you need to know
https://www.medicalnewstoday.com/articles/322715.php Most women need to wait at least 6 weeks before having sex after a C-section, or until their doctor or midwife says it is safe. They may also need to take a few precautions and make some adjustments to their sexual activities in the short term. A C-section, also known as a cesarean delivery, involves a doctor delivering a baby through a long incision in the abdomen instead of through the vagina. An estimated one in four pregnant women will undergo cesarean delivery, and questions about how it affects postpartum sexual activity are very common. In this article, we address some common concerns, including how long to wait, what to expect, and if there will be an increased risk of bleeding. How long to wait While there is no standard amount of time a woman should wait before returning to regular sexual activities following cesarean delivery, it is best to wait until a doctor says it is safe. Most women get the OK from doctors at their 6-week postnatal checkup and may choose to start having sex after this point. In a 2013 study that included more than 1,500 women, 53 percent had attempted sexual activity within 6 weeks of giving birth. Of these women, 41 percent had tried vaginal sex. Everyone's recovery is different, and the pace may depend on whether the cesarean delivery was extensive or unplanned. Many women who have undergone cesarean delivery chose to wait at least 4–6 weeks before having sex because they experience soreness, vaginal bleeding, and fatigue following the birth. Women should also avoid wearing tampons until postpartum bleeding, or lochia, is complete. Precautions After a doctor says that it is safe to try sexual activity, people may still need to take some precautions to reduce the risk of complications. There may be some soreness and swelling around the incision site, and the surrounding skin may feel tight or stretched. As the incision site heals, it will also be more prone to tearing, so it is essential to avoid strenuous activities, including some sexual activities. It is best to avoid lifting anything heavier than the baby. There is also usually heavy bruising along and around the incision site, and this will slowly fade in the weeks following the surgery. A doctor may remove the surgical staples before a woman leaves the hospital, but the abdomen will still be very sore and tender for a few weeks. The vagina usually feels wider, swollen, or bruised after giving birth. The cervix also needs time to heal and return to its regular size before a person can start having sex or using tampons again. Anyone who has recently undergone a cesarean delivery should watch out for signs of infection and other complications. These signs include: a fever over 100.4° F severe pain leaking urine heavy vaginal bleeding, such as bleeding that soaks a maxi pad in 1 hour large clots bad-smelling discharge oozing from the incision severe or continual bleeding from the incision swelling around the incision site swelling or pain in the lower legs pain when peeing vomiting, diarrhea, or nausea shortness of breath hives or a rash an intense headache that comes on suddenly and does not go away unexplained anxiety, depression, or panic flu-like symptoms What to expect Many women do not feel like having sex for a few weeks or months after giving birth, either vaginally or by cesarean delivery. There is no need to rush. Most women and their partners are exhausted from taking care of a newborn, so sex may not rank high on the list of priorities. It is essential to keep in mind that sex should be pleasurable. If sexual activity causes any pain or discomfort, it is best to stop. If the incision site is sore, try positions that do not put any pressure on the woman's abdomen. Hormonal changes after birth may lead to vaginal dryness, so it may be a good idea to use a lubricant. If penetration is uncomfortable or painful, it can help to focus on nonpenetrative activities. Some types of foreplay, such as massage, can also help people to relax and enjoy their experience. It is crucial to keep in mind that everyone heals differently. If sexual activity becomes more painful over time, talk to a doctor. Authors of one study reported that the rate of sexual problems in first-time mothers rose from 38 percent before pregnancy to 83 percent in the first 3 months following delivery. This figure declined to 64 percent 6 months after birth. In one cohort study, the researchers found no differences regarding sexual problems after delivery among women who gave birth vaginally and those who underwent cesarean delivery. However, results of another cohort study suggested that women who had undergone cesarean delivery were more likely to delay having sex longer than those who had given birth vaginally. Is there an increased risk of bleeding? After giving birth, all women experience a period of vaginal bleeding called lochia. This bleeding continues until the uterus shrinks back to its regular size. Lochia causes bright red blood to leak from the vagina. Most women wear extra-absorbent pads or padded underwear during this time. Lochia bleeding eventually changes from bright red to dark red or pale pink. Over time, it fades to an orange or yellowish color. Activity levels can also affect this period of bleeding. If the amount of blood suddenly increases, it may mean that a woman is doing too much too quickly after surgery. For 1 or 2 weeks after cesarean delivery, a woman may also notice some periodic, minor bleeding from the incision site. Strenuous activity, including sex, can increase the risk of opening the incision or experiencing a blood clot. Birth control after giving birth Technically, a woman can get pregnant as soon as 3 weeks after giving birth, regardless of whether they are breast-feeding. Women can even get pregnant after giving birth if they have not yet had a period. This means that women who may become pregnant through sexual intercourse usually wish to use birth control. Many women return to their preferred method of birth control. It is best to speak to a doctor or nurse about the best methods before leaving the hospital or during the 6-week checkup. Recovery Most women need to spend 3–4 days recovering in the hospital after cesarean delivery. After 24 hours, a doctor or nurse will often recommend getting up and gently moving around, even just to go to the bathroom. A nurse may also demonstrate ways of moving that are less likely to cause pain from the incision site. A doctor may leave the dressing on the incision site for at least 24 hours after the surgery. Most cesarean delivery incisions are between 10 and 20 centimeters long. They run horizontally across the abdomen, usually just above the underwear line. Before a woman leaves the hospital, the doctor will give instructions to ensure that the wound heals properly and remains free from infection. Takeaway There is no right time to begin having sex again after cesarean delivery. However, the cervix needs time to heal, and the incision site will be more prone to infection in the initial weeks, so it is best to wait until a doctor says it is safe. A doctor will usually give the go-ahead close to the 6-week checkup, but many women prefer to wait longer. Take things slowly and communicate what feels pleasurable and what does not. If sex is painful, it is essential to say so. People may choose to stop or try a different position or activity. If sex becomes more painful over time instead of less, speak to a doctor. |
|
#182
|
||||
|
||||
|
Re: Sexual Health News
What is labial hypertrophy and is it normal?
https://www.medicalnewstoday.com/articles/322755.php Labial hypertrophy is the medical term for when one or both of the vaginal lips or labia is larger than usual. Having enlarged labia is normal and not a cause for concern. Many people are born with large and often asymmetrical labia and experience no negative side effects. People can have surgery to safely change the shape of the labia, though this is not usually necessary. Is labial hypertrophy normal? Labial hypertrophy describes the enlargement of the vaginal lips. The labia help cushion the inner vagina and clitoris from friction, impact, and damage. The size and shape of people's genitals vary significantly from person-to-person. The vaginal lips, or labia, are often asymmetrical, and it is normal for each side to have its own shape. The outside of the vagina, which is called the vulva, contains: the labia majora or outer lips or skin folds the labia minora or inner lips or skin folds Labial hypertrophy can affect both sets of labia, but it is more likely to change the labia minora or inner lips. Hypertrophy in the labia majora may cause them to appear enlarged. Hypertrophy in the labia minora may cause them to stick out past the labia majora. Labial hypertrophy is harmless. It does not impact a person's sexual health and does not mean they have an underlying medical condition. Many people have labial hypertrophy without knowing it, and most do not experience adverse symptoms. Side effects of labial hypertrophy Most people with labial hypertrophy will not have any additional symptoms or side effects. In others, enlarged labia may cause discomfort or put them at risk for other issues. Possible side effects include: Discomfort or irritation The labia are a sensitive area, and longer labia may become irritated more easily. Some people with enlarged labia may feel discomfort when doing physical activities that add friction or pressure to the vaginal area, such as horseback riding or cycling. They may also notice pain from friction during sexual activity. Enlarged labia may rub against a person's underwear, causing persistent irritation to this sensitive area. Keeping clean A person who has labial hypertrophy will often have additional areas of folded skin around the vulva. This makes it especially important to thoroughly clean the area when washing, as there are more areas for bacteria to become trapped. People should always wash their hands before touching the sensitive vaginal area to prevent the transfer of bacteria. It is essential to wash the area well if it becomes itchy or irritated. Incorrect vaginal hygiene can make people more susceptible to bacterial growths and yeast infections. Causes There is no known direct reason for labial hypertrophy. Doctors see it as a natural fluctuation in the human body. Just as one breast may be larger than the other, differences in the labia are usual. Some people are born with enlarged labia, while it may develop over time due to hormonal fluctuations in others. In some people, the labia become larger as they go through puberty. Some people also notice that their labia grow after pregnancy, while others see changes in their vulva with age. Diagnosis Diagnosing labial hypertrophy is simple. A physical examination by a doctor or gynecologist is usually all that is required. There is no standard of measurement for how large labia should be. Treatment In most cases, people do not need treatment. However, if labial hypertrophy causes physical or psychological discomfort, there are treatment options, as follows: Lifestyle changes Some people with labial hypertrophy may notice that their discomfort goes away if they stop wearing tight clothing or underwear. Wearing loose-fitting underwear, shorts, and pants may help prevent unnecessary friction in the area. Wearing natural materials, such as cotton or linen, may also help improve airflow around the vulva. Doctors may also be able to provide women with topical ointments to reduce irritation or manage symptoms. Other tips to help manage possible symptoms include: Choose natural, unscented tampons or menstrual pads, avoiding any additional ingredients or chemicals. Wear a protective pad or use a cushioned seat when doing physical activities that may irritate the labia, such as cycling. Practice good hygiene and wash with a hypoallergenic soap that is free from harsh chemicals or perfumes. Surgery Some people may choose to have surgery to reduce the size of their labia. This involves a procedure called a labioplasty. A labioplasty is typically done for cosmetic reasons and involves removing excess skin and reshaping the labia to be more symmetrical. The surgery usually requires general anesthesia. The surgery may cause bruising or swelling in the vulva, as it heals. The vulva will also be very delicate during the healing process. People will need to take extra care to keep the area clean and dry to avoid infections or bleeding. Doctors may also advise people to avoid friction and wear loose clothing while the labia recover. Surgery always carries risks, such as having a reaction to anesthesia or developing scar tissue. Doctors will discuss these risks and a person's other options before continuing with any treatment. Doctors will give specific instructions to people about when they can resume physical and sexual activity. Is labioplasty safe in teens? Surgeons may also perform a labioplasty on teenagers going through puberty who may be developing enlarged labia. However, because the labia may still be growing, doctors usually advise people to wait until after puberty before having surgery. Doctors will talk through labial hypertrophy with teens to help them understand that it is a normal change in the body. They will also talk about the emotional and mental health factors involved in cosmetic surgery. Outlook Labial hypertrophy is usual in individuals and, in many cases, causes no adverse side effects. Surgery is an option in severe cases or cases that cause emotional discomfort. The outlook for surgery is generally good and has a very high satisfaction rate. Doctors may have additional tips about soothing irritation or managing effects of hypertrophy, and many people find they can relieve any discomfort by making a few lifestyle changes. |
|
#183
|
||||
|
||||
|
Re: Sexual Health News
side effects of birth control pills and why can the birth control pill make your breasts bigger?
https://www.medicalnewstoday.com/articles/322758.php Birth control pills contain hormones, and they can increase a person's breast size. However, the effect is usually temporary. The two primary hormones present in most types of birth control pill are: estrogen, a female sex hormone progestin, a synthetic version of progesterone, which is another female sex hormone The body produces estrogen and progesterone. During the menstrual cycle, levels fluctuate, and this can cause a change in breast tissue. Estrogen is also the hormone primarily responsible for the development of breasts during puberty. When a person starts taking the birth control pill, their levels of these hormones rise, and this can result in an increase in breast size. However, the size of the breasts may return to normal after a few monthly cycles or after a person stops taking the pill. Can birth control affect breast size and how? Birth control pills can increase the size of a person's breasts. Estrogen and progesterone levels change during the menstrual cycle, and this can cause changes in the breast tissue. A person may feel that their breasts are tender or sore, as a result. Many birth control pills contain the same hormones, estrogen and progestin, which is a synthetic form of progesterone. Starting to take the pill can stimulate the breasts to grow. However, any increase in size is typically slight. Within a few months of taking the pill, the breasts generally return to their regular size. This usually also happens if a person stops taking the pill. There is another link between the birth control pill and breast enlargement. When a person starts taking birth control, the changes to hormone levels can cause the body to retain fluid. This can make the breasts feel engorged. When fluid retention, or edema, is responsible for breasts that feel bigger, a person may notice that their breast size returns to normal during the week that they are not taking an active pill. During this week, they will get a period. Can birth control make people gain weight? Weight gain is a side effect of many birth control pills. Like the possible increase in breast size, any associated weight gain is typically slight. In 2014, researchers published a review of 49 trials. They had tried to find a causal link between weight gain and types of birth control that contained both estrogen and progestin. The researchers found that these pills tended to have no significant impact on weight. If a person who starts taking the birth control pill does experience minor weight gain, it is because hormonal changes have caused the body to retain fluid. Other side effects of birth control In general, doctors consider the pill to be safe. However, a person should be aware of some possible side effects, which include: changes in mood changes in menstruation, involving either more or less bleeding tenderness in the breasts nausea headaches The increase in hormones, particularly estrogen, can also cause more serious side effects. Birth control pills that only contain progestin are less likely to cause these effects. Serious, though rare, side effects of birth control include: blood clots stroke heart attack Before starting or changing a method of birth control, discuss the risks with a doctor. When to see a doctor A person must see a doctor before they can start taking the birth control pill and before switching pills. It is essential for each person to discuss the potential side effects and risk factors with a medical professional. Some risk factors to consider include: being overweight or obese smoking being over the age of 35 having a history of migraines with auras having a history of high blood pressure the presence of a clotting disorder having high cholesterol If a person has any of these risk factors, a doctor may recommend a different type of birth control. The doctor should be able to provide additional options. Takeaway When taking a birth control pill, a person should be aware of the potential risks and side effects. One of the milder side effects is a slight, temporary increase in breast size. Though rare, some other side effects are more severe, and they can even be life-threatening. Before a person starts using hormone-based birth control, it is essential to discuss the advantages and disadvantages with a doctor. |
|
#184
|
||||
|
||||
|
Re: Sexual Health News
Foods to eat for better sex
https://www.medicalnewstoday.com/articles/322779.php Humans have looked for ways to improve their sexual experience for thousands of years, including trying to discover the best foods for sex. Scientists have linked a variety of foods with better sex. In this article, learn about which foods to eat to boost libido, improve stamina, and enhance your sex life. Foods for circulation and stamina Keeping the circulatory system in good working order is essential for sexual health. Better circulation can lead to an improved sexual response in men and women. This is especially true for the erectile response. Cardiac health is also vital for stamina. In other words, if it is good for the heart, it is good for a person's sex life. The American Heart Association recommend a diet that includes: a wide range of fruits and vegetables whole grains and plenty of fiber healthful oils, such as olive oil and sunflower oil seafood, nuts, and legumes Research suggests that following this heart-healthy diet can improve certain aspects of sexual health. Researchers studying the Mediterranean Diet, which follows similar lines to the American Heart Association's, found that people with metabolic syndrome who followed the diet had fewer problems with erectile dysfunction, otherwise known as ED. Also, many of the foods featured in a heart-healthy diet, such as avocados, asparagus, nuts, seafood, and fruit, have associations with better sex in both traditional medicine and scientific research. For example, in Nahuatl — the language once used by the Aztecs — the term for avocados was the same as the term for testicles. Also, researchers found that people who ate avocados had a reduced risk of metabolic syndrome, which is a risk factor for ED. Men with metabolic syndrome are almost twice as likely as men without it to experience ED, so adding healthful fats, such as those in avocados, to a varied diet may help. Foods to boost libido Foods that can help people improve their libido are commonly called aphrodisiacs, after Aphrodite, the ancient Greek goddess of love. Oysters are among the most famous aphrodisiacs in history. Their effects may be due to their zinc content. Zinc is a mineral the body needs every day for many vital functions, such as cell metabolism, stamina, and regulating levels of testosterone. Testosterone is the most important male sex hormone. One older study found that zinc might be helpful for treating ED in people with chronic kidney disease. Oysters have more zinc than any other food per serving. Some examples of other foods that are high in zinc are: crab lobster red meat fortified breakfast cereal pine nuts However, sexual desire is complex and has to do with many more factors than just nutrition, including an individual's relationships, stress levels, and personal preference. It is natural for people to experience ups and downs in their interest in sex. Many alternative healthcare practitioners claim diet can help. While more scientific research is needed, the following foods are possible libido-boosters: Asian and American ginseng Fenugreek Maca Foods to help maintain an erection When a person has difficulty getting and maintaining an erection, doctors refer to it as ED. According to the Urology Care Foundation, ED affects up to 30 million men in the United States. Understanding the physical, mental, and emotional factors that contribute to ED can help people choose a diet that promotes better sex. Factors that contribute to ED include: problems with blood flowing into and staying in the penis damage to nerve centers in the penis side effects of medication, radiation, and other medical treatments depression, anxiety, and stress Tackling the underlying cause is the best way to treat ED. But another thing people can do is eat more fruit. In one study, researchers linked a higher fruit intake to a 14 percent reduction in the risk of ED. The flavonoid content of many fruits may be responsible for this improvement. Foods rich in flavonoids include: berries citrus fruits grapes apples hot peppers cocoa products red wine tea (green, white, and black) Research in an animal model has also shown that watermelon may be effective against ED. The melon's content of the amino acid l-citrulline may explain this positive action. Also, nitric oxide may be beneficial to prevent ED by increasing blood flow and vasodilation. Beets also contain nitrates, which convert to nitric oxide and may be beneficial for blood flow. Takeaway Many people look to their diet to increase their sexual desire, improve their ability to have sex, and increase the pleasure they get from sex. While research indicates possible links between particular foods and better sex, those seeking the best food for sex should ensure they are eating a balanced, heart-healthy diet. |
|
#185
|
||||
|
||||
|
Re: Sexual Health News
I noticed this too that each time if my diet consists of veggies, i somehow perform much better in the bedroom
|
|
#186
|
||||
|
||||
|
Re: Sexual Health News
Long-lasting HIV injection is a step closer after second GSK study
https://www.reuters.com/article/us-g...-idUSKCN1N42CP LONDON (Reuters) - A once-monthly injection to control HIV proved as effective as daily pills in a second study by GlaxoSmithKline, paving the way for a new regimen that could be simpler for some patients to be filed with regulators. The experimental two-drug injection of cabotegravir and rilpivirine was shown to suppress the HIV virus in a cohort of adults who had not been on a long-established daily three-drug oral regimen, GSK’s majority-owned HIV unit ViiV Healthcare said. In the study, adults with HIV were first put on a 20-week three-drug program of daily tablets to suppress the virus before being switched to monthly injections. After 48 weeks, the injections maintained a similar rate of suppression as the pills, it said. The results support an earlier major study, which involved adults who had been using a three-drug oral regimen to control the virus. ViiV Healthcare’s chief medical officer John C. Pottage said the trial provided further evidence that a long-acting injection could offer an alternative to daily, oral therapy for people who had previously achieved viral suppression. “This innovative dosing regimen could transform HIV therapy by reducing the number of days a person receives treatment from 365 to 12,” he said. “Work on new methods of HIV treatment, including long-acting injectable therapies, supports our goal of making HIV a smaller part of the lives of people living with HIV.” ViiV Healthcare, which is also owned by Pfizer and Shionogi, hopes that its work on developing two-drug therapies will help it compete against Gilead Sciences, the U.S. drugmaker that dominates the $26 billion-a-year HIV market. The company said detailed results of the study would be presented at an upcoming scientific meeting. |
|
#187
|
||||
|
||||
|
Re: Sexual Health News
Online tool can help men make prostate cancer treatment choices
Read more at https://www.channelnewsasia.com/news...oices-10952258 A web-based tool can let a man with prostate cancer see how thousands of other men in his situation have chosen to be treated, which may help him better understand his own options, a US study suggests. Early-stage prostate cancer may not need treatment right away, or ever, because these tumors often don't grow fast enough to cause symptoms. Because treatment can have side effects like impotence and incontinence, doctors sometimes advise men to put off surgery or radiation and instead get regular screenings to reassess whether the cancer warrants intervention. "There is often no one correct treatment option because the choice of prostate cancer treatment depends on personal preferences around treatment benefits and risks," said senior author Dr Karandeep Singh of the University of Michigan in Ann Arbor. "There are already a number of great resources available to the prostate cancer patient community to support this shared decision-making process," Singh said by email. "However, there are no tools that help patients discover what treatments similar men chose when faced with a similar decision." Singh and colleagues set out to develop a tool that fit the bill. They used data on treatment choices made by 5,016 men diagnosed with prostate cancer to develop a web-based tool that predicts the most likely treatment choice based on what other men in similar circumstances have chosen. Then, they asked another 2,527 men with prostate cancer to try out the tool and see how often the program predicted the treatment choice these men would pick for themselves. The tool, it turned out, was highly accurate. "This tool is not meant to replace the shared decision-making process but rather to augment that process by helping patients focus their preparation on likely treatment options prior to meeting with their urologist," Singh said. Patients and doctors can use the tool here: https://bit. ly/2Kjprcw It's only meant for men with early-stage tumors that haven't spread to other parts of the body. It won't predict treatment decisions for men with more complex cases. For men who do have early-stage tumors, the tool focuses on aspects of the prostate cancer diagnosis, patients' age and weight, and any history of heart attack or diagnosis of diabetes. When men are only 45 years old with lower-risk tumors, they will probably see that similar patients are pretty evenly divided between opting for radical prostatectomy surgery and choosing active surveillance, that is, skipping treatment in favor of periodic reassessments to see if cancer warrants intervention. By age 55, men with low-risk tumors might see that more than half of similar patients choose active surveillance and less than 40 per cent opt for a radical prostatectomy. And by 65, men with low-risk tumors might see that about two-thirds of similar patients pick active surveillance. One limitation of the study is that it wasn't designed to prove whether or how the web-based tool might help men make treatment decisions or see how happy patients are afterwards with the choices they made, the study authors note. Even when men seem similar on paper in terms of their demographics and the particulars of their tumor, how well the web-based tool predicts what's best for them might vary from one man to the next, said Dr. Kari Tikkinen of the University of Helsinki and Helsinki University Hospital in Finland. "Sure, this data can be reassuring to those whose own values and preferences concur with the option machine learning is suggesting as the most common choice," Tikkinen, who wasn't involved in the study, said by email. "However, even in this kind of excellent situation it may not help patients," Tikkinen said. A man who is very opposed to surgery because of the risk of incontinence or impotence, for example, may not want to choose surgery just because that's what the tool says most similar men would do, Tikkinen said. But tools like the one tested in the study can still help men have more focused and nuanced conversations with their doctors about what treatment may be ideal for them, Tikkinen said. SOURCE: https://https://bit. ly/2Bm8MlN European Urology, online October 11, 2018. Read more at https://www.channelnewsasia.com/news...oices-10952258 |
|
#188
|
||||
|
||||
|
Re: Sexual Health News
Scientists believe people should be eating less meat and more vegetables
https://www.news.com.au/lifestyle/he...dbfd20fdf4b3b0 Scientists have unveiled what they say is an ideal diet for the health of the planet and its people — including a doubling of consumption of nuts, fruits, vegetables and legumes, and a halving of meat and sugar intake. If the world followed the Planetary Health diet, the researchers said, more than 11 million premature deaths could be prevented each year, while greenhouse gas emissions would be cut and more land, water and biodiversity would be preserved. “The food we eat and how we produce it determines the health of people and the planet, and we are currently getting this seriously wrong,” said Tim Lang, a professor at Britain’s University of London who co-led the research. Feeding a growing population of 10 billion people by 2050 with a healthy, sustainable diet will be impossible without transforming eating habits, improving food production and reducing food waste, he said. “We need a significant overhaul, changing the global food system on a scale not seen before.” Many life-threatening chronic diseases are linked to poor diets, including obesity, diabetes, malnutrition and several types of cancer. The researchers said unhealthy diets currently cause more death and disease worldwide than unsafe sex, alcohol, drug and tobacco use combined. It suggested cutting back meat consumption to 14g a day The proposed planetary diet is the result of a three-year project commissioned by The Lancet health journal and involving 37 specialists from 16 countries. It says global average consumption of foods such as red meat and sugar should be cut by 50 per cent, while consumption of nuts, fruits, vegetables and legumes should double. For individual regions, this could mean even more dramatic changes: People in North America, for example, eat almost 6.5 times the recommended amount of red meat, while people in South Asia eat only half the amount suggested by the planetary diet. Meeting the targets for starchy vegetables such as potatoes and cassava would need big changes in sub-Saharan Africa, where people on average eat 7.5 times the suggested amount. The researchers said they acknowledged it was very ambitious to hope to get everyone in the world to adopt it, not least because there is vast global inequality of access to food. “More than 800 million people have insufficient food, while many more consume an unhealthy diet that contributes to premature death and disease,” said Walter Willett of Harvard University. |
|
#189
|
||||
|
||||
|
Re: Sexual Health News
Quote:
Eggs twice a week max and all coffee and tea has been replaced with Turmeric and Almond milk. It has made a huge difference. Less fat, more muscle, better sleep and higher energy levels.
__________________
Tips for ALL samsters.
|
|
#190
|
||||
|
||||
|
Re: Sexual Health News
Safest condoms and methods of use
https://www.medicalnewstoday.com/articles/323089.php Condoms are an effective method for preventing pregnancy and sexually transmitted infections. Most brands are very safe, but some offer less protection than others. Condoms are a popular barrier method of conception. Condoms made of latex, polyisoprene, or polyurethane effectively prevent pregnancy and the transmission of certain sexually transmitted infections (STIs). Most commercial brands of condoms are very safe and approved by the U.S. Food and Drug Administration (FDA). However, people should look out for novelty condoms and natural condoms, which may not offer the same levels of protection. In this article, we look at which condoms are safest and provide tips for using condoms to make sure they are effective. How safe are condoms for pregnancy and STIs? Male condoms are considered a safe and overall effective form of birth control. According to Planned Parenthood, condoms are 98 percent effective at preventing pregnancy when used correctly. If used incorrectly, the effectiveness rate drops to about 85 percent. By contrast, female condoms are 95 percent effective when used correctly. When people do not use them correctly, this figure drops to 79 percent. Both male and female condoms also provide protection against STIs that are transmitted through bodily fluids, including semen, vaginal fluid, and blood. Condoms act as a barrier for all of these fluids and can protect against infections such as: gonorrhea chlamydia HIV syphilis Condoms do not protect as effectively against some other STIs, such as herpes and genital warts. These infections re transmitted through skin-to-skin contact affecting the labia, scrotum, and inner thighs, and condoms only cover the shaft of the penis or the inside of the vagina or anus. Safest condoms and methods Most condoms are very safe. The FDA require all latex and polyurethane condoms to undergo quality testing. They require manufacturers to spot-check their products. Additionally, the FDA collects random condom samples from warehouses, and fill these with water to check for leaks. At least 996 of every 1,000 condoms must pass the water leak test before the FDA consider them safe for use. People can use the following advice to make sure they are using the right condoms in the safest possible way: 1. Avoid novelty condoms Many manufacturers have designed novelty condoms for stimulation rather than protection. Avoid brands that do not mention STI or pregnancy protection. If a condom does not cover the entire penis, it will not provide complete protection. 2. Read the packaging Look for a statement on the label that indicates the condom will prevent STIs. Several brands, including Trojan and Duralex, offer varieties of condoms that can help prevent STIs. However, as mentioned above, condoms do not protect against all STIs. People may still contract an STI that someone transmits through skin-to-skin contact. People should always read the label carefully and read up on specific brands to confirm whether the condom meets all safety standards. 3. Avoid natural condoms Natural condoms are a long-standing alternative to latex condoms. They are effective for preventing pregnancy, but they often do not protect against STIs. People with latex allergies, or those looking for an alternative to latex, should instead try polyurethane condoms. These are slightly more expensive but offer a looser fit and the same protection as latex condoms against STIs and pregnancy. 4. Use lubricated condoms Not everyone needs to use extra lubrication. The vagina naturally produces lubrication when a person is aroused. However, sometimes this lubrication is not enough. In these cases, people should either use lubricated condoms or a separate water-based or silicon-based lubricant. Lubrication on the outside of the condom reduces friction during sex and helps prevent the condom from either slipping off or breaking during sex. 5. Do not use oil-based lubricant Oils, such as baby oil, lotions, or petroleum jelly, can cause the condom to break, and people should not use these with condoms. 6. Do not use expired condoms Condoms have an expiration date written on their packaging. If a condom is past its expiration date, a person should throw it away, as it will be more likely to break than a newer one. 7. Avoid condoms that were not stored correctly Condoms are affected by heat and friction, so the way people store them is important. Always store condoms in a cool, dry place, as they can break down in extreme hot or cold temperatures. Storing condoms in an extreme temperature environment can weaken a condom and make it less effective. People should not store condoms in their wallet, as they can be exposed to friction and heat which can cause weakness or tears. 8. Avoid condoms with spermicide Some condoms contain spermicide. The FDA has approved nonoxynol 9 (N-9) as an over-the-counter spermicide. For some people, this spermicide may cause vaginal or anal irritation. For others, this may not be an issue. Tips for using condoms safely Condoms — as is the case with all birth control — are only effective when used correctly. Always check the condom's expiration date and inspect the packaging to make sure there are no holes or tears. Store them away from direct sunlight and extreme temperatures. When using a condom, a person should follow these basic safety steps: Always check the packaging for the date and tears. Open the package carefully and avoid using sharp instruments, including teeth. Put the condom on after the penis becomes erect, but before it comes in contact with the vagina or anus. Pinch the tip before unrolling the condom over the penis. Use water-based lubrication on the outside of the condom to prevent tears or the condom slipping off. Grip the base of the condom after ejaculation and remove from vagina or anus before the penis becomes flaccid. Wrap the condom in a tissue and throw it out after use. Always use a new condom for each sexual encounter. For female condoms, people should follow these additional steps: Guide the penis into the opening of the condom. Pinch the opening together when removing the condom from the vagina. What to do if a condom breaks If a condom breaks during intercourse, stop immediately and remove the broken condom. If there is any risk of an STI, people should see their doctor, as soon as possible. The doctor will do a sexual health screening and advise about how to look for signs of STIs if they appear. If people are worried about pregnancy, there are a number of emergency contraception options available from doctors, sexual health clinics, or over the counter at a pharmacy. People can choose between emergency contraception pills or an intrauterine device (IUD). These can help prevent pregnancy when used early after a condom breaks. The sooner a person takes emergency contraception, the more effective it is. Advantages and disadvantages of condoms Both males and females condoms are available. Male condoms are typically more affordable and have more varieties. Male condoms can vary in shape, size, flavor, and color. Both male and female condoms are highly effective in preventing pregnancy and STIs when used correctly. Both male and female condoms have some advantages and disadvantages that people should consider when deciding on birth control. Advantages of condoms include the following: less costly than hormonal methods and may be available free at certain health clinics non-hormonal way of working available in places that do not have a pharmacy protect against STIs where most other forms of birth control do not There are also certain disadvantages of condoms compared with other methods of contraception, such as the following: there is a chance a condom will break improper usage makes them less safe oil-based lubricants can break down latex condoms Takeaway Condoms are an overall reliable and safe choice for people to use for protected sex. Unlike some other forms of birth control, most condoms offer additional protection from STIs. Condoms created for use in the U.S. must pass safety standards, so much of choosing the right condom comes down to personal preferences. |
|
#191
|
||||
|
||||
|
Re: Sexual Health News
Typical testosterone levels in males and females
https://www.medicalnewstoday.com/articles/323085.php The amount of testosterone a person has in their body can vary throughout their life. Levels depend on a person's age, sex, and health. Males usually have much higher levels of testosterone in their body than females. Testosterone is a hormone known as an androgen. Although primarily known as a male sex hormone, females also need certain levels of testosterone. However, most testosterone converts into the sex hormone estradiol in the female body. In males, the testes produce testosterone, and the ovaries produce testosterone in females. The adrenal glands also produce small amounts of testosterone in both sexes. Testosterone in males is important for: development during puberty sperm creation strengthening of muscles and bones sex drive Testosterone in females is essential for: maintaining levels of other hormones sex drive and fertility making new blood cells There is a link between low testosterone and sex drive and fertility for both sexes. The body controls testosterone levels naturally and having low testosterone levels is more common than having high testosterone levels. Typical testosterone levels Doctors measure testosterone in nanograms per deciliter (ng/dl). The following tables show healthy levels of total testosterone in the body. Levels fall within a range for each age bracket. People will have different levels of testosterone within this healthy range. Infants and children 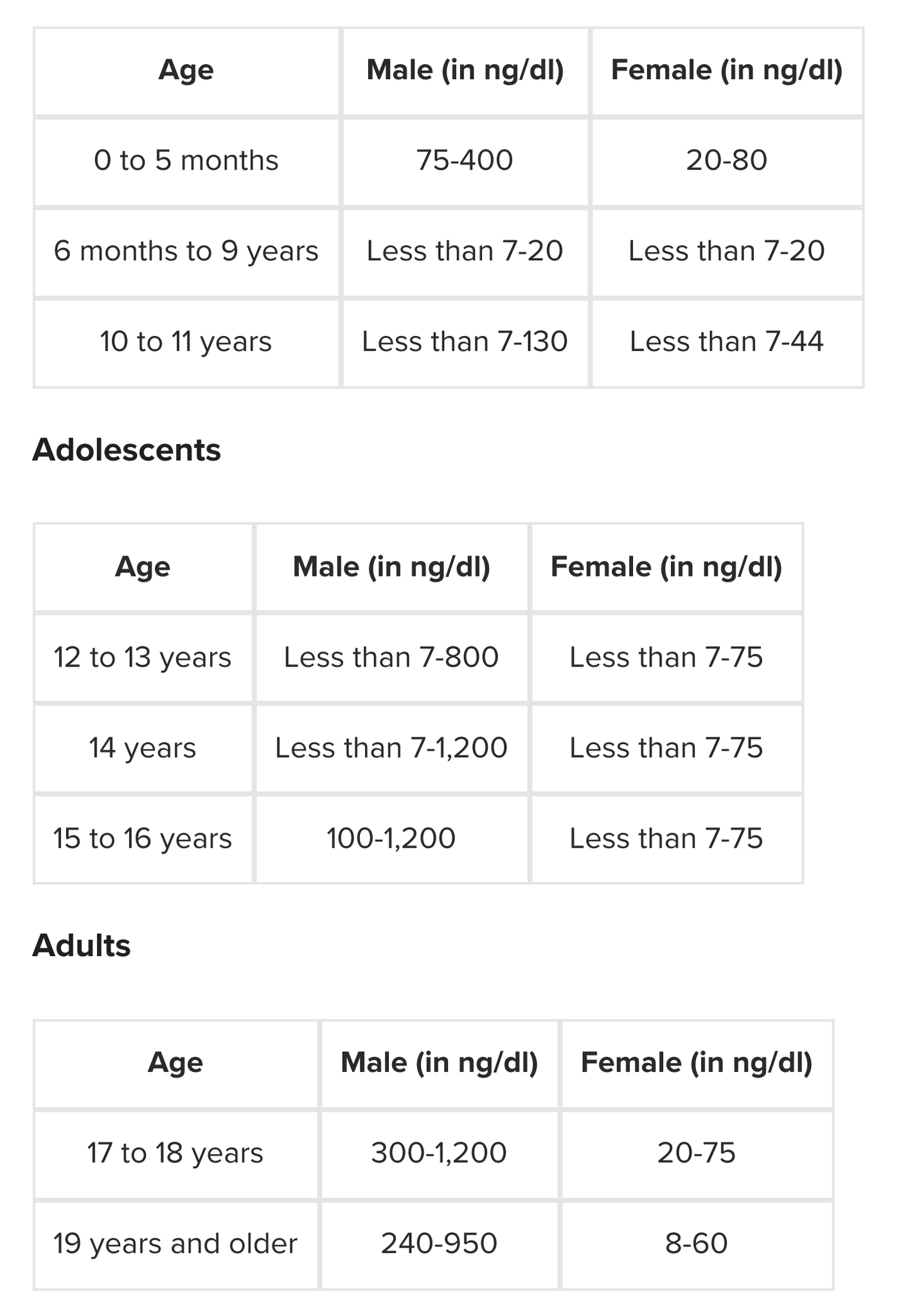 Doctors may also measure testosterone alongside Tanner staging. The Tanner scale tracks the visual development of children during puberty according to five fixed stages rather than a person's specific age. For example, stage II of the Tanner scale relates to the growth of a boy's testicles or the development of breast buds in a girl, but it does not refer to their actual age. Because hormone levels change rapidly during puberty and development can happen at different ages for different people, the Tanner scale is a more accurate way to judge changes during puberty than referring to age. According to the Tanner scale, healthy testosterone levels are as follows: 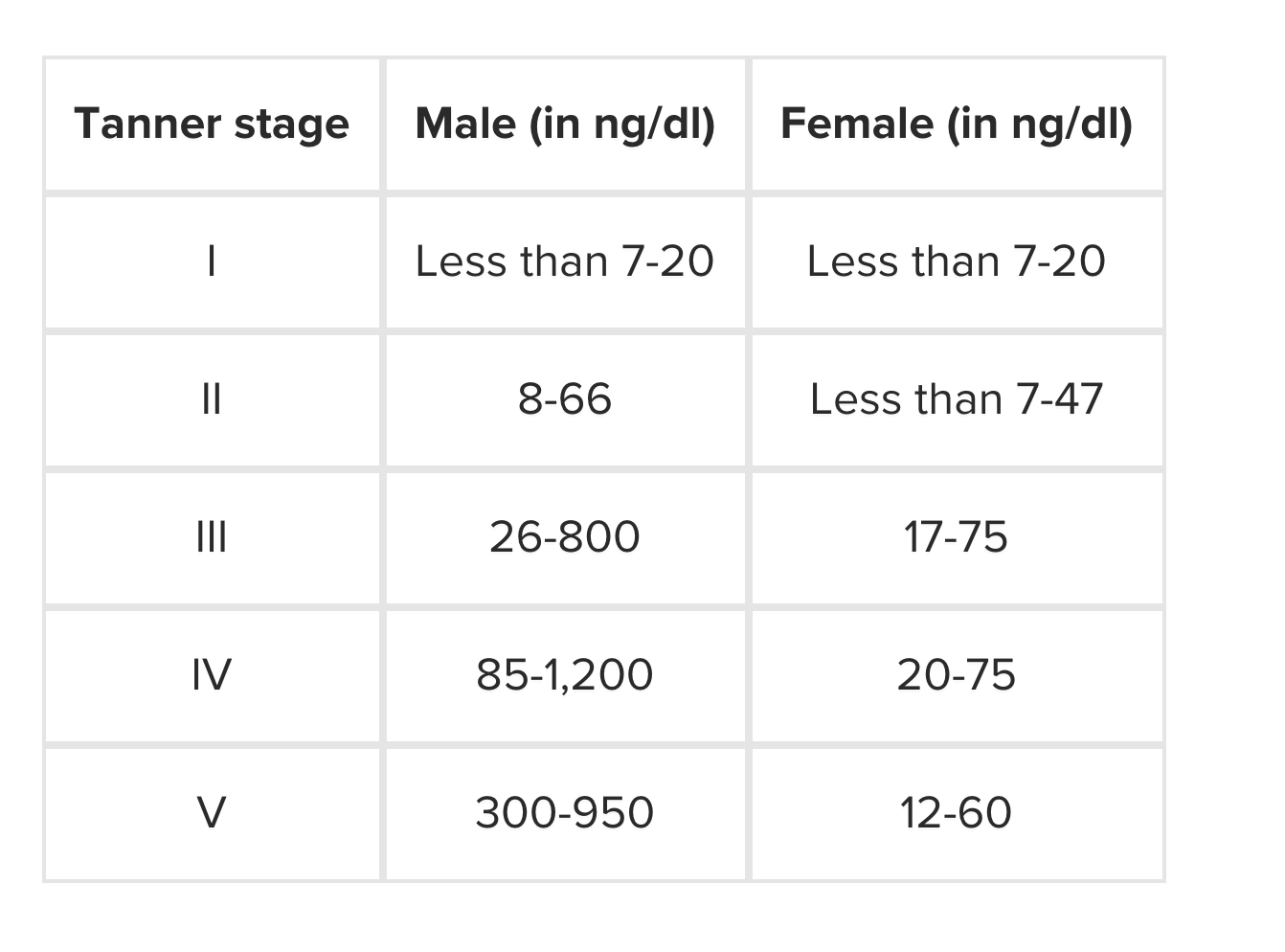 Low testosterone levels A testosterone deficiency in the womb can affect the development of a male fetus. It can also affect male puberty, and it may slow or stop a person's growth or development. Hormone levels change for both males and females as they age. Females experience a more dramatic change in hormones, with levels falling until a female reaches menopause. Males experience a more gradual change in hormone levels. Testosterone levels decrease naturally with age in both sexes. In males, lower testosterone levels can lead to: hair loss (including on the body and face) reduced muscle tone more fragile skin a reduced sex drive disturbed mood memory or concentration problems Low testosterone levels in females can lead to: irregular or missed periods low sex drive vaginal dryness weak bones fertility problems However, more research into the effects of low testosterone on the body as people age is needed. High testosterone levels High testosterone levels are unusual in adult males. Children with high testosterone levels may have a growth spurt or start puberty early. High testosterone in both sexes can cause infertility in some cases. Polycystic ovary syndrome Polycystic ovary syndrome (PCOS) affects females. It occurs when the ovaries produce too much testosterone. Symptoms include: irregular or no periods oily skin acne increased hair growth on the face, back, or chest It is not clear what causes PCOS, but researchers think it is a combination of genes and environment. Steroid use Steroids have similar properties to testosterone, and some people use them to build muscle or gain weight. However, steroids can affect testosterone levels in both males and females. If a person takes too many steroids, it can raise the levels of testosterone in their blood, causing the body to stop producing testosterone. In males, this excess of testosterone can also lead to a decrease in the amount of sperm that the body makes, which may lead to infertility or loss of sex drive. For females, steroids can cause a deeper voice, male pattern baldness, irregular periods, and may lead to infertility. Both males and females may experience hair growth on the face and body, greasy skin, and a range of other symptoms. Testing and diagnosis Anyone who suspects that their testosterone levels are high or low should see their doctor or get tested. To diagnose low or high testosterone, a doctor will ask about a person's medical history, do a physical examination, and order some tests. In males, a doctor might: discuss any use of steroids or opiates talk about a person's development at puberty measure their BMI and waist size check hair for any pattern of baldness check the size of the testicle and prostate gland In females, a doctor will usually need to check or ask questions about: menstruation acne or skin conditions body or facial hair muscle bulk For adolescents, a doctor will look for signs of puberty. Total testosterone level test The total testosterone level test is a blood test. The best time to have the test is in the morning when levels of testosterone in the blood are usually highest. However, testosterone levels vary throughout the day, so some people may need to have the test again to confirm the result. Treatment options and takeaway Treatment will depend on the underlying health condition. It is possible to treat males for low testosterone levels with an injection or prescription gel. People using this treatment long-term could experience potentially severe side effects, such as an increased risk for heart problems. Females who develop PCOS might be able to treat their symptoms with weight loss, hormonal contraception , and fertility treatment if needed. |
|
#192
|
||||
|
||||
|
Re: Sexual Health News
What can make urination painful?
https://www.medicalnewstoday.com/articles/323105.php A condition affecting the bladder or nearby parts of the body can cause painful urination. Doctors may also refer to painful urination as dysuria. Multiple potential causes for this symptom exist, and many of them are treatable. People with dysuria should make their doctor aware of any other symptoms that they are experiencing. If these relate to the painful urination, it can help doctors make a diagnosis and recommend appropriate treatment. Causes of dysuria Many different conditions can cause painful urination. Most of these causes are highly treatable. Below are 10 possible causes of painful urination, along with other symptoms that may occur alongside it. 1. Urinary tract infection A urinary tract infection (UTI) occurs when excess bacteria build up somewhere in the urinary tract. This part of the body runs from the kidneys to the bladder to the urethra, which carries urine toward the outside of the body. Additional symptoms A person with a UTI may experience other symptoms, such as: needing to urinate frequently passing cloudy or blood-tinged urine fever foul-smelling urine pain in the side and back 2. Sexually transmitted infection Sexually transmitted infections (STIs), such as chlamydia, gonorrhea, and herpes, can all affect the urinary tract and lead to pain when urinating. Additional symptoms Symptoms may vary according to the type of STI. For example, herpes typically causes blister-like lesions on the genitals. 3. Prostate infection A short-term bacterial infection can result in a prostate infection or prostatitis. Chronic inflammation from another condition, such as an STI, can also cause prostatitis. Additional symptoms A prostate infection may also cause: difficulty urinating pain in the bladder, testicles, and penis difficulty ejaculating and painful ejaculation needing to urinate frequently, especially at night 4. Kidney stones Kidney stones are collections of materials, such as calcium or uric acid, that build up and form hardened stones in and around the kidneys. Sometimes, the kidney stones will lodge themselves near the area where urine enters the bladder. This can cause painful urination. Additional symptoms In addition to dysuria, kidney stones can cause the following symptoms: pain in the side and back pink- or brown-tinted urine cloudy urine nausea vomiting pain that changes in intensity fever chills urinating only small amounts frequently 5. Ovarian cysts Much like kidney stones, ovarian cysts are an example of how something outside the bladder can press on it and cause painful urination. Ovarian cysts can develop on one or both ovaries, which sit on either side of the bladder. Additional symptoms People with ovarian cysts may experience: unusual vaginal bleeding pelvic pain difficulty recognizing that the bladder is empty after urinating painful periods breast tenderness a dull ache in the lower back 6. Interstitial cystitis Also known as bladder pain syndrome, interstitial cystitis is a condition that causes chronic irritation of the bladder lasting 6 weeks or more without an underlying infection. Additional symptoms Interstitial cystitis may also cause the symptoms below: pressure in the bladder area pain during intercourse pain in the vulva or vagina pain in the scrotum urinating frequently but producing little urine 7. Chemical sensitivity Sometimes, chemicals that are external to the body, such as fragrances, can irritate bodily tissues. When a person urinates, this irritation may be more noticeable, and pain may occur. Products that can cause chemical sensitivity include: douches soaps scented toilet paper vaginal lubricants contraceptive foams Additional symptoms People who react to chemical products may notice: swelling redness itching irritation of the skin on or around the genitals 8. Vaginal infection or irritation Also known as vaginitis or vaginosis, a vaginal infection can occur due to the overgrowth of bacteria or yeast. An STI called trichomoniasis can also cause a vaginal infection. Additional symptoms The following symptoms may occur alongside painful urination: foul-smelling or unusual vaginal discharge vaginal irritation pain during intercourse vaginal bleeding, which is usually mild 9. Medication Some medications, including those that doctors prescribe to treat bladder cancer, may irritate and inflame the bladder tissues. This can often cause pain when urinating. If a person has started a new medication and begins to feel pain when urinating, they should call their doctor and ask if the symptom may be a side effect of the drug. They should not stop taking the medication on their own without asking a doctor first. Additional symptoms Additional symptoms vary based on the type of medication. 10. Bladder cancer Bladder cancer occurs when cancer cells start to develop in the bladder. Feeling pain when urinating is not typically an early symptom of this condition. Instead, a person usually notices blood in their urine. Additional symptoms Other possible symptoms of bladder cancer include: frequent urination having difficulty urinating or passing a weak urine stream lower back pain appetite loss weight loss fatigue foot swelling bone pain Differences in males and females Males and females can both experience pain when urinating, and the causes may be anatomy-dependent. For example, females have shorter urethras than males. As a result, bacteria can often enter the bladder more easily, which can lead to UTIs. A person can talk to their doctor about their risks for painful urination based on their sex as well as their medical history. When to see a doctor Everyone may experience painful urination from time to time. A person should see their doctor if the pain is consistent, and they are also experiencing the following symptoms: blood in the urine, which will usually appear pink, brown, or red pain in the side or back pain that lasts longer than 24 hours unusual discharge from the penis or vagina fever If an adult has a fever that is higher than 103°F, they should seek emergency medical attention. A person should not ignore pain when urinating. A doctor can often help identify treatments that will reduce pain. Potential treatment options Treatment options for painful urination depend on the underlying cause. Some examples include: Treating UTIs with antibiotics. Severe UTIs that affect the kidneys may require intravenous antibiotics. Treating prostatitis with antibiotics. A person may take these for up to 12 weeks if they have chronic bacterial prostatitis. Other possible prostatitis treatments include over-the-counter (OTC) anti-inflammatories, prostatic massage, hot baths, and medications called alpha-blockers, which relax the muscles around the prostate. Avoiding the use of harsh soaps or other chemical products near the genitals that could potentially lead to irritation. A person's symptoms will often resolve quickly when chemical irritation is the underlying cause. At-home care for painful urination often includes taking OTC anti-inflammatory medications, such as ibuprofen. A doctor will often encourage a person to drink more fluids as this dilutes urine, making it less painful to pass. Resting and taking medications as directed can usually help relieve most symptoms. Summary Painful urination is a common symptom with many causes, several of which are related to bacterial infection. People who feel ill should see their doctor before an infection has time to get worse and cause additional symptoms. |
|
#193
|
||||
|
||||
|
Re: Sexual Health News
What to know about HPV and fertility
https://www.medicalnewstoday.com/articles/323512.php Human papillomavirus or HPV is the name for a group of viruses transmitted by skin-to-skin contact. HPV can affect fertility in both men and women. It is the most common sexually transmitted infection (STI), but people can also acquire it in other ways. According to the United States' Centers for Disease Control and Prevention (CDC), 80 percent of people will have an HPV infection at some point in their life, many without realizing. Doctors consider different strains of HPV either low- or high-risk. The two most high-risk strains of HPV are HPV 16 and HPV 18, which are more likely to cause serious complications, such as cancer. In general, however, 90 percent of HPV infections clear up without treatment within 2 years, without causing any adverse effects. In this article, learn about how HPV may affect fertility in both men and women. HPV and women's fertility In general, research shows that any infection, including HPV, makes it more difficult for a woman to conceive and remain pregnant. However, it is important to remember that most cases of HPV clear up without any need for treatment. The American College of Obstetricians and Gynecologists (ACOG) list scarring and blockages in the fallopian tubes as potential risk factors for infertility. This type of damage can sometimes be due to STIs, such as HPV, but the ACOG do not list HPV as a specific contributor to infertility. How much HPV influences a woman's fertility still needs more study. Women with HPV may experience: Difficulties getting pregnant: HPV may reduce the embryo's ability to implant itself in the wall of the womb or uterus. HPV infections can also damage the embryo. Increased risk of miscarriage: There is a link between HPV and the risk of pregnancy loss and spontaneous preterm birth, but these risks depend on the type of HPV a person has contracted. Studies show a significant association between cervical HPV infections and pregnancy loss. It is vital to remember that the body's immune system clears most HPV infections without any additional treatment. HPV and men's fertility HPV can also affect fertility in men. According to a 2018 study, the presence of HPV in sperm negatively affects pregnancy outcomes, either by contributing to infertility or increasing the risk of pregnancy loss. Men with fertility issues are 3 to 4 times more likely than other men to have HPV. The HPV virus affects fertility in men by binding with the head of the sperm cell, which hinders the sperm cell's ability to move freely. How does HPV affect pregnancy? HPV in men, women, or both can negatively affect the pregnancy outcome by increasing the risk of pregnancy loss. Assisted reproductive technologies (ART) For people using assisted reproduction, research shows that HPV-positive couples may have more difficulties getting and remaining pregnant, using intrauterine insemination (IUI) or in vitro fertilization (IVF), than HPV-negative couples. A 2018 systematic review found that in cases where the male partner had HPV, it negatively affected pregnancy rates and increased the risk of miscarriage. One 2016 study found that HPV-positive women were six times less likely than HPV-negative women to become pregnant after using IUI. Prevention There are several ways to reduce the likelihood of contracting HPV. Get vaccinated: HPV vaccines are highly effective for both men and women, and provide close to 100 percent protection against several types of HPV and genital warts. Make sure partners are vaccinated: Sexual partners can easily transfer HPV between each other. If one partner has HPV, it is likely that the other partner will get it. Making sure partners are vaccinated can help prevent transmission. Practice safe sex: Using condoms reduces the risk of getting and transferring HPV. However, condoms are not as effective at preventing HPV infection as they are at preventing the spread of other STIs, as HPV can affect areas not covered by a condom. Get regular Pap smears: Regular Pap smears help screen for HPV, including strains that may increase the risk of cervical precancer and cancer. HPV-positive? Get vaccinated anyway: One study showed a positive association between vaccination and higher pregnancy rates and lower rates of miscarriage, even in people who already had HPV. Other risks of HPV Some strains of HPV, particularly HPV 16 and HPV 18 are known risk factors for cancer. Research found that people had HPV in 96 percent of cervical cancer cases and 93 percent of anal cancer cases. People with certain strains of HPV may have a higher risk of developing the following types of cancer: cervical anal throat mouth genital Summary Getting vaccinated is the best way to prevent HPV. If vaccination is not possible, or if a person already has HPV, practicing safe sex or choosing vaccinated partners helps to reduce risks. If a person or couple is having fertility issues, they may wish to speak to a doctor about HPV testing. Even if they already have HPV, vaccination may help improve fertility and pregnancy outcomes. However, in most cases, HPV clears up without treatment and will not cause any lasting effects, including fertility issues. The complications of HPV depend on the particular strain. People with HPV should know which strain they have and become familiar with the risks to help avoid HPV-associated cancers. |
|
#194
|
||||
|
||||
|
Re: Sexual Health News
Dental dams: Everything you need to know
https://www.medicalnewstoday.com/articles/323768.php It is possible to pass a sexually transmitted infection to a partner through oral-genital or oral-anal sex. A device known as a dental dam can be effective in reducing this risk. A dental dam is a barrier between a person's mouth and another person's genitals. Many people use them during oral sex. Dental dams consist of a square of thin material, usually latex or polyurethane. Dental dams come in a variety of colors and with or without lubricant. Some dental dams are flavored. What do they protect against? Dental dams protect against the spread of sexually transmitted infections (STIs) or other germs, such as E. coli, during oral sex. They prevent the mouth from coming into contact with the vagina, vulva, and anus. People can transmit several STIs during oral sex, including: chlamydia gonorrhea syphilis HIV There is little research on how effective dental dams are but, similarly to condoms, people must use them properly and consistently for full protection. It is possible to transmit other infections, such as herpes simplex type 1 and 2, human papillomavirus (HPV), and pubic lice (crabs). A person can get genital herpes from an infected partner during oral sex if they have not entirely covered the outbreak or lesion. It is also possible to catch pubic lice from a partner, even while using a dental dam. Depending on the type of contact, it is possible to get an STI infection in the throat, mouth, anus, rectum, genitals, or even the urinary tract. Often, a person with an STI in their throat or mouth does not have any symptoms other than a sore throat. How to use a dental dam Dental dams are easy to use. Simply unroll the dental dam and place it over the vulva or anus before performing oral sex. Make sure to use the dental dam during the entire session, from start to finish. People should only use dental dams over the vulva or anus. When performing oral sex on a man, a person should use a condom instead of a dental dam. Here are a couple of tips for using a dental dam: Use a water-based lubricant. Avoid using oil-based products, such as petroleum jelly, lotion, or oil, as these can make the dam less effective. Apply the lubricant between the dam and the skin to prevent irritation. Avoid spermicides or nonoxynol-9 products. These substances can increase the risk of irritation to the mouth or throat. Only use a dental dam once. Be sure to use a fresh one for each instance of oral sex. Store correctly. Double check expiration dates and keep the dams in a cool, dry place. Look out for allergies to latex. Opt for a polyurethane dam if either partner is allergic to latex. Throw away damaged dams. If the dam gets crinkled or rips during oral sex, throw it out and use a new one. Making a homemade dental dam 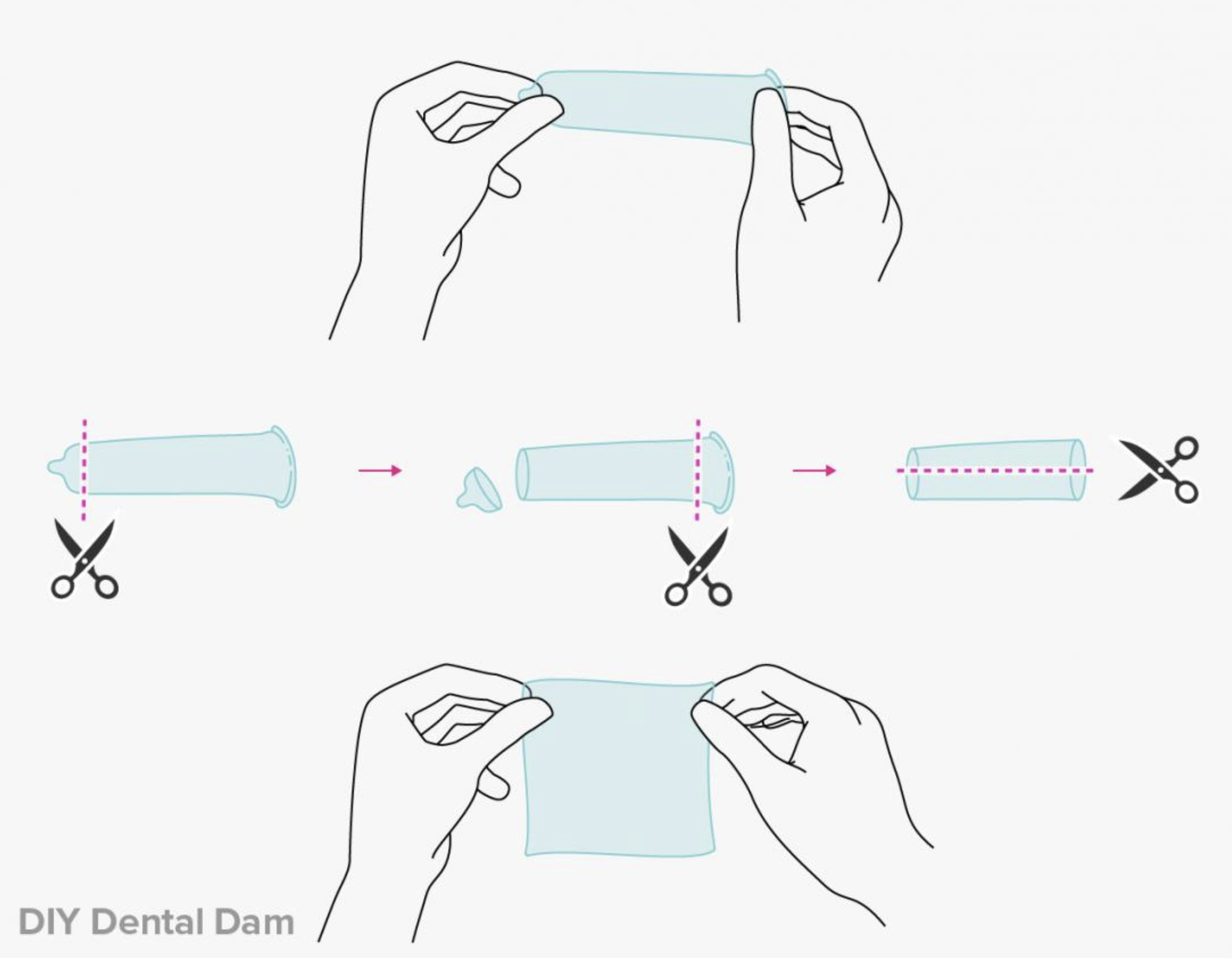 Image credit: Diego Sabogal. If a person has a condom, they can just cut the tip and elastic at the base, then make another cut down the length of the condom and open it up into a square. Another option is to use a sheet of kitchen plastic wrap. Plastic wrap is not designed for this purpose but can add protection if a person does not have access to a condom. Plastic wrap is readily available in many grocery stores, and a person can use it with either water- or oil-based lubricants. However, plastic wrap is delicate and can rip easily. Finally, there are single-use oral sex latex panties available, but these have yet to get approval from the United States Food and Drug Administration for this purpose. While the single-use panties are more expensive than other options, they may feel more comfortable than a dental dam. Takeaway It is possible to transmit STIs through oral sex. Many people are not aware that they have an STI of the throat or mouth because there are often no symptoms. Dental dams can provide a vital layer of protection during oral sex, especially among nonmonogamous couples or those with an active STI. Dental dams are available at pharmacies, sexual health clinics, and online. |
|
#195
|
||||
|
||||
|
Re: Sexual Health News
What causes pelvic pain in women?
https://www.medicalnewstoday.com/articles/323796.php Pelvic pain affects the lowest part of the abdomen, between the belly button and groin. In women, pelvic pain may be a sign of menstrual cramps, ovulation, or a gastrointestinal issue such as a food intolerance. It can also develop due to a more serious problem. Sometimes, pelvic pain is an indicator of an infection or issue with the reproductive system or other organs in the area. When this is the case, a woman may need to see a doctor. In this article, we look at 15 possible causes of pelvic pain in women. Causes 1. Menstrual pain and cramps Menstrual pain and cramping are a common cause of pelvic pain in women. Of all menstrual disorders, women most commonly report experiencing pain, say the American College of Obstetricians and Gynecologists (ACOG). Over half of women who menstruate will experience some pain for at least 1–2 days each cycle. Menstrual cramping will typically occur immediately before a woman starts her period, as the uterus contracts and sheds its lining. The pain may feel similar to a muscle spasm or a jabbing pain. Using a warm heat pad may relieve the sensation. Over-the-counter medications, such as ibuprofen (Advil) and naproxen (Aleve), may also help relieve pain. In cases of severe pain from menstruation, doctors can recommend other medications. 2. Ovulation If a woman feels a painful sensation on one side of her pelvis in the middle of her menstrual cycle, she may be experiencing mittelschmerz. Doctors use this German word to describe painful ovulation. When a woman ovulates, the ovaries release an egg, along with some other fluid. The egg will then travel down the fallopian tube and into the uterus. The fluid released by the ovary can spread within the pelvic area, sometimes, causing irritation in the pelvis and leading to pain. The discomfort may last for minutes or hours, and it may switch sides of the body, depending on which ovary released the egg. The pain is temporary and requires no specific treatment. 3. Interstitial cystitis It is also possible for a woman to experience ongoing bladder inflammation that has no known cause. The medical term for this is interstitial cystitis, and doctors are currently unsure why it happens. Interstitial cystitis can cause pelvic pain and symptoms such as painful urination, needing to urinate frequently, and pain during sex. Treatment often involves managing symptoms as best as possible. 4. Cystitis or urinary tract infections Cystitis refers to inflammation in the bladder due to a bacterial infection. This happens because vaginal, rectal, or skin bacteria can enter the urethra and make their way to the bladder. A urinary tract infection (UTI) is one that can occur anywhere in the system, while cystitis occurs only in the bladder. Both conditions are common in women. These infections will sometimes clear up on their own, but a short course of antibiotics will typically treat cystitis and other UTIs. 5. Sexually transmitted infections Pelvic pain may indicate the presence of a sexually transmitted infection (STI) such as gonorrhea or chlamydia. STIs occur in people who are sexually active. Chlamydia affects around 2.86 million people each year in the United States, according to the Centers for Disease Control and Prevention (CDC). The CDC also estimate that gonorrhea affects 820,000 people every year. Along with pelvic pain, other symptoms of STIs may include painful urination, bleeding between periods, and changes in vaginal discharge. Anyone experiencing these changes should see their doctor who will be able to diagnose an STI and prescribe treatment, usually including antibiotics. It is also critical to inform sexual partners about the infection to prevent it from spreading. 6. Pelvic inflammatory disease Pelvic inflammatory disease (PID) is an infection in the womb that can damage the surrounding tissue. PID can arise if bacteria from the vagina or cervix enter the womb and take hold. It is usually a complication of an STI such as gonorrhea or chlamydia. Along with pelvic pain, women may experience other symptoms, including abnormal vaginal discharge and bleeding. PID increases a woman's risk of infertility. The CDC note that 1 in 8 women who have had PID also have trouble becoming pregnant. Treatment typically involves taking antibiotics to treat the bacterial infection. However, they cannot treat scarring, which is why early treatment is crucial. 7. Endometriosis Endometriosis occurs when endometrium, or tissue that lines the inside of the uterus, grows outside of the womb. Endometriosis may be a source of chronic, long-lasting pelvic pain in some women. When a person's period begins, this tissue outside of the uterus responds to hormonal changes, which may cause bleeding and inflammation in the pelvis. Some people may experience mild to severe pain. Endometriosis may make it difficult for some women to become pregnant. Doctors may recommend various treatments, depending on symptom severity. 8. Irritable bowel syndrome Irritable bowel syndrome (IBS) is a gut disorder that causes pain and symptoms, including constipation, diarrhea, and bloating. The symptoms of IBS tend to flare up and go away over time, especially after a bowel movement. There is no cure for IBS, so treatment focuses on managing symptoms through changes in diet, stress levels, and medications. 9. Appendicitis Appendicitis is inflammation in the appendix, which is a small organ in the lower-right abdomen. An infection causes this condition, and, although it is common, it can be severe. Anyone experiencing a sharp pain in their lower-right abdomen, along with other symptoms such as vomiting and fever, should seek immediate medical care, as this may be a sign of appendicitis. 10. Urinary stones Stones in the urinary tract consist of salts and minerals, such as calcium, that the body has trouble getting rid of in the urine. These minerals can build up and form crystals in the bladder or kidneys that often cause pain in the pelvis or lower back. Stones may also cause the urine to change color, often turning it pink or reddish with blood. Some stones do not require treatment, but passing them can be painful. At other times, a doctor may recommend medications to break up stones or surgery to remove them. 11. Ectopic pregnancy An ectopic pregnancy occurs when an embryo implants itself anywhere outside of the uterus and starts growing. A woman may feel very sharp pain, and cramps in her pelvis, which are usually focused on one side. Other symptoms include nausea, vaginal bleeding, and dizziness. Anyone who suspects that they have an ectopic pregnancy should seek immediate medical care, as this is a life-threatening condition. 12. Pelvic adhesions An adhesion is scar tissue that occurs inside the body and connects two tissues that should not be connected. This may result in pain, as the body struggles to adapt to the adhesion The scar tissue could form due to an old infection, endometriosis, or other issues in the area. Pelvic adhesions may lead to chronic pelvic pain in some women, and they may cause other symptoms, depending on where the scar tissue appears. A doctor may recommend some minimally invasive surgeries to help reduce adhesions and relieve symptoms. 13. Ovarian cysts Ovarian cysts occur when the ovaries fail to release an egg. The follicle holding the egg may not open completely to release the egg, or it may become clogged with fluid. When this happens, a growth called a cyst forms in the area, which may cause bloating, pressure, or pelvic pain on the side of the body with the cyst. As the ACOG explain, most cysts are noncancerous. In many cases, ovarian cysts go away on their own. In some cases, a cyst may bleed or burst, which can cause sharp, severe pain in the pelvis and may require medical treatment. Doctors can identify ovarian cysts using ultrasound, and they may recommend treatments that range from watchful waiting to surgery. 14. Uterine fibroids Fibroids are lumps of muscle and fibrous tissue within the uterus. While they are noncancerous and do not tend to cause symptoms, these growths can be a source of pain. They may cause discomfort in the pelvis or lower back or pain during sex. Fibroids may also cause excessive bleeding or cramping during menstruation. Some fibroids do not require treatment. If a woman finds her symptoms difficult to manage, doctors may recommend one of many treatments, including medications, noninvasive procedures, or surgery. 15. Tumor In rare cases, a malignant growth in the reproductive system, urinary tract, or gastrointestinal system may be the reason for pain in the pelvis. The tumor may also cause other symptoms, depending on where it appears. Doctors will need to perform a thorough evaluation, often using blood and imaging tests, to identify a tumor. Once they have diagnosed the issue, they will recommend possible treatments. When to see a doctor For many causes of pelvic pain, it is not necessary to seek medical care. However, there are some occasions when the woman should see a doctor. Any new, severe pain requires evaluation. For example, a person who suspects that an infection is causing their pelvic pain should visit a doctor. While some infections clear up on their own, the chance of complications is often not worth the risk of waiting. Anyone with vaginal bleeding they do not expect, and severe pain should also consult a doctor promptly. If a person has a known condition and experiences sudden changes in pain, such as sharp twists or sudden severe pain, they should seek medical attention, as this could be a sign of a serious change in the condition. Other symptoms that appear alongside pelvic pain, such as fever, nausea, and vomiting, are also signs that someone should see a doctor. They will make a thorough evaluation and help devise a suitable treatment plan. Summary For the most part, pelvic pain in women appears as a result of a common issue such as menstrual cramping or painful ovulation. However, if a person notices signs that a more serious underlying problem is causing the pain, they should consider seeing a doctor. A thorough diagnosis is essential in every case so that people can avoid potentially serious complications and find the best treatment. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |