 |
|
#841
|
|||
|
|||
|
Re: All you need to know about HIV
Does sucking pussy transmit hiv?
|
|
#842
|
|||
|
|||
|
Re: All you need to know about HIV
It is theoretically possible.
Vaginal secretions contain HIV virus. HIV virus can penetrate the lining of the inside of the mouth (buccal mucosa). However, there are also several theories to explain why we have never seen a case of HIV infection via cunnilingus. 1. HIV Virus is richer in cervical secretions which are deep in the vagina compared to extrenal secretions. 2. The saliva contains chemicals and antibodies that can inactivate the HIV virus 3. The saliva is too dilute for HIV virus to survive. Practically speaking, I would go so far as to say that there is zero risk of HIV infection from cunnilingus. |
|
#843
|
|||
|
|||
|
Re: All you need to know about HIV
had a protected sex but bbbj with a lady from rws.how high is my risk from getting hiv
|
|
#844
|
||||
|
||||
|
Re: All you need to know about HIV
Quote:
However your risk of Herpes, Syphilis, Gonorrhea, Chlamydia etc will be high if the lady is infected with any of these diseases.
__________________
Tips for ALL samsters.
|
|
#845
|
||||
|
||||
|
Re: All you need to know about HIV
|
|
#846
|
||||
|
||||
|
Re: All you need to know about HIV
Bro. Why not go for a test at DSC? I had the same worry but decided to go ahead for a full check at DSC. Costs $122 for peace of mind. I was.glad I did. The wait of about 1 week for results gave me some time to reflect my foolishness.
|
|
#847
|
||||
|
||||
|
Re: All you need to know about HIV
Quote:
http://std.about.com/od/riskfactorsf...Prostitute.htm Question: What Are the Risks of Having Oral Sex Performed by a Prostitute? Once a month or so, I receive an e-mail from a man who has visited a prostitute for a blow job and wants to know what the risks of oral sex are. These questions are often from men who have visited high-risk prostitutes outside the U.S.; however, that generally only changes the magnitude of the risk, not the nature of it. Unprotected fellatio is potentially risky for any man who receives it, not just for those who visit prostitutes and other commercial sex workers. Answer: The risks of oral sex are numerous. Unprotected oral sex can spread a variety of STDs, including herpes, syphilis, HPV, gonorrhea, and rarely, HIV. Men who visit prostitutes in the developing world and other high-risk areas are often particularly concerned about contracting HIV through oral sex. HIV can be transmitted through oral sex, although the risk of contracting HIV is much higher during other forms of sexual activity. However, since oral sex does include a risk of HIV, it is always a good idea to use a condom during oral sex -- particularly with an untested partner or a partner who is high-risk, such as a prostitute. Condoms are very effective at reducing HIV risk. HIV is not the only potential negative consequence of receiving a blow job from a prostitute or other partner. Syphilis and gonorrhea can both be transmitted during a blow job, as can HPV and herpes. As with HIV, practicing safe oral sex will reduce your risk -- although condoms may not be 100 percent effective at preventing the diseases that can be spread from skin to skin. Under no circumstances should you simply wait to see if you develop symptoms to determine whether your sexual encounter has exposed you to an STD. Many men with STDs never show any obvious symptoms, but they can still suffer long-term health effects or pass the infections onto their partners. Fortunately, except for HPV, all of the above diseases can be screened for using blood or urine testing, but it may take several months to be certain that your results are reliable. A lot of men want me to quantify their level of risk after they've received an unprotected blow job from a prostitute. The problem is that there's no practical way to do so. The most accurate answer I can give is that it is possible that they've been exposed to and infected with one or more of the STDs described above, and the only way to be certain is to get tested. Furthermore, since blood tests that are antibody based can take a few months to produce reliable results, they should consider the possibility that they are putting their sexual partners at risk during future sexual encounters and discuss their risk and practice safe sex accordingly.
__________________
Tips for ALL samsters.
|
|
#848
|
|||
|
|||
|
Re: All you need to know about HIV
Dear bros,
On 2nd Sep I had a session with a fl (thai) by the name Alice from pataya1baby. My condom broke while I ejaculate inside her. I was scared as hell and went to take pep at dsc the next day. However, after 5 days of taking, I was too sick by the side effects that I stopped. I msg okt abt this matter and he said the 21 yrs old thai is recently new in this stable. He said no one feedback to him about condom break except me from the her arrival date on 22nd aug 2015 till 5 sep 2015. I'm still worried sick and couldn't sleep until my next appt with dsc on 16th sep. I will do a full course test just to be safe I don't pass anything to my wife and children. Anyone got similar exp they care to share? Or someone has encounter with this alice before? |
|
#849
|
||||
|
||||
|
Re: All you need to know about HIV
Quote:

__________________
Tips for ALL samsters.
|
|
#850
|
|||
|
|||
|
Re: All you need to know about HIV
I mean if anyone had sex with alice and contracted stis or hiv?
|
|
#851
|
||||
|
||||
|
Re: All you need to know about HIV
Quote:

__________________
Tips for ALL samsters.
|
|
#852
|
||||
|
||||
|
Re: All you need to know about HIV
Treat all people living with HIV, offer antiretrovirals as additional prevention choice for people at "substantial" risk
New policies could help avert more than 21 million deaths and 28 million new infections by 2030 http://www.who.int/mediacentre/news/...mmendation/en/ 30 SEPTEMBER 2015 ¦ GENEVA - Anyone infected with HIV should begin antiretroviral treatment as soon after diagnosis as possible, WHO announced Wednesday. With its "treat-all" recommendation, WHO removes all limitations on eligibility for antiretroviral therapy (ART) among people living with HIV; all populations and age groups are now eligible for treatment. The expanded use of antiretroviral treatment is supported by recent findings from clinical trials confirming that early use of ART keeps people living with HIV alive, healthier and reduces the risk of transmitting the virus to partners. WHO now also recommends that people at "substantial" risk of HIV should be offered preventive antiretroviral treatment. This new recommendation builds on 2014 WHO guidance to offer a combination of antiretroviral drugs to prevent HIV acquisition, pre-exposure prophylaxis (PrEP), for men who have sex with men. Following further evidence of the effectiveness and acceptability of PrEP, WHO has now broadened this recommendation to support the offer of PrEP to other population groups at significant HIV risk. PrEP should be seen as an additional prevention choice based on a comprehensive package of services, including HIV testing, counselling and support, and access to condoms and safe injection equipment. New recommendations on early use of ART and expanded offer of PrEP are contained in WHOs "Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. The new guideline stresses that, in order to effectively implement the recommendations, countries will need to ensure that testing and treatment for HIV infection are readily available and that those undergoing treatment are supported to adhere to recommended regimens and are retained in care. The recommendations were developed as part of a comprehensive update of the "WHO consolidated guidelines on the use of antiretroviral drugs for preventing and treating HIV infection". This early release guideline is shared ahead of the full publication, slated for release later this year, because of their potential for public health impact. Based on the new recommendations, the number of people eligible for antiretroviral treatment increases from 28 million to all 37 million people who currently live with HIV globally. Expanding access to treatment is at the heart of a new set of targets for 2020 with the aim to end the AIDS epidemic by 2030. These targets include 90% of people living with HIV being aware of their HIV infection, 90% of those receiving antiretroviral treatment, and 90% of people on ART having no detectable virus in their blood. According to UNAIDS estimates, expanding ART to all people living with HIV and expanding prevention choices can help avert 21 million AIDS-related deaths and 28 million new infections by 2030. |
|
#853
|
||||
|
||||
|
Re: All you need to know about HIV
http://www.who.int/mediacentre/factsheets/fs360/en/
Key facts updated Updated July 2015 HIV continues to be a major global public health issue, having claimed more than 34 million lives so far. In 2014, 1.2 [1.01.5] million people died from HIV-related causes globally. There were approximately 36.9 [34.341.4] million people living with HIV at the end of 2014 with 2.0 [1.92.2] million people becoming newly infected with HIV in 2014 globally. Sub-Saharan Africa is the most affected region, with 25.8 [24.028.7] million people living with HIV in 2014. Also sub-Saharan Africa accounts for almost 70% of the global total of new HIV infections. HIV infection is often diagnosed through rapid diagnostic tests (RDTs), which detect the presence or absence of HIV antibodies. Most often these tests provide same day test results; essential for same day diagnosis and early treatment and care. There is no cure for HIV infection. However, effective treatment with antiretroviral (ARV) drugs can control the virus so that people with HIV can enjoy healthy and productive lives. It is estimated that currently only 51% of people with HIV know their status. In 2014, approximately 150 million children and adults in 129 low- and middle-income countries received HIV testing services. In 2014, 14.9 million people living with HIV were receiving antiretroviral therapy (ART) globally, of which 13.5 million were receiving ART in low- and middle-income countries. The 14.9 million people on ART represent 40% [3745%] of people living with HIV globally |
|
#854
|
||||
|
||||
|
Re: All you need to know about HIV
New single-tablet HIV treatment wins FDA approval
http://www.medicalnewstoday.com/articles/302153.php The US Food and Drug Administration have approved a new single tablet as a complete treatment for the treatment of HIV-1 infection in people aged 12 years and over. The new treatment, called Genvoya, from Gilead Sciences, is a fixed-dose combination of elvitegravir, cobicistat, emtricitabine and tenofovir alafenamide. It is intended for patients aged 12 and over, weighing at least 35 kg (77 lbs) and who have never been treated for HIV before, or for infected adults whose HIV is currently suppressed. The drug was tested against other HIV treatments approved by the Food and Drug Administration (FDA) in four clinical trials involving a total of 3,171 participants. Results showed that it reduced viral loads and was comparable to other treatments. Genvoya contains a new version of tenofovir - a powerful HIV inhibitor - that has not been approved before. Gilead say that because the new version (called TAF) enters cells - including HIV-infected cells - more efficiently than the previous version (TDF), it can be given at a lower dose that results in 91% less tenofovir in the bloodstream. The new drug was developed to reduce side effects, and the trial results show it appears to be associated with less kidney toxicity and reductions in bone density than previously approved drugs containing tenofovir. Read more |
|
#855
|
||||
|
||||
|
Re: All you need to know about HIV
What is PrEP?
http://afa.org.sg/portfolio-item/prep-answered/ PrEP stands for Pre-Exposure Prophylaxis, a daily oral regimen of 2 drugs Tenofovir and Emtricitabine; prescribed a single fixed-dose combination tablet to prevent HIV transmission. It is to be differentiated from PEP or Post exposure prophylaxis where the person takes a 3-drug regimen within 72 hours after a possible exposure to HIV for 28 days. PrEP is an additional preventive tool for sexually active gay men who are at high risk of HIV acquisition; it is NOT meant to replace condoms, but to supplement them. PrEP does not prevent other sexually transmitted infections viz. syphilis, gonorrhoea, infections with Chlamydia, herpes simplex, hepatitis B and C etc. Learn how HIV Medication works Is PrEP effective? Strict medication adherence is critical to PrEP efficacy. In a study involving gay men (the iPREX study), PrEP was associated with an average 44% reduction in HIV acquisition. However, the protection can be up to 92% if medication was detectable in the blood of persons in the trial (compared to those with no detectable medication in the blood) At current times, it is recommended that PrEP be taken on a daily basis. What is the time line to achieving protection? The time from initiation of medications to maximal protection again HIV is unknown. Drug levels are seen at rectal tissues by 7 days and maximum intracellular drug levels are seen at 20 days of daily oral dosing . What laboratory tests do I need to do before and after starting PrEP? PrEP should be prescribed from a healthcare setting. A baseline HIV test must be performed at least 3 months from the last high-risk sexual exposure. The test MUST be negative before starting PrEP. Subsequently HIV tests must be done every 3 months to exclude acute HIV infections. Taking PrEP when you are newly infected with HIV is very dangerous. This is because you will be under-treated, this will lead to resistant HIV strains that will make future treatment more challenging. Medications for PrEP can hurt the kidneys. Baseline tests for kidney function have to be assessed and monitored every 6 months. Screening for other STIs is also recommended at regular intervals. Baseline Hepatitis B screening is also recommended as Tenofovir has activity against the virus and the doctor will need to monitor liver function tests. What is Acute HIV infection? Many people develop this illness a few weeks after being infected with HIV. This is possible if there is suboptimal adherence to daily PrEP. 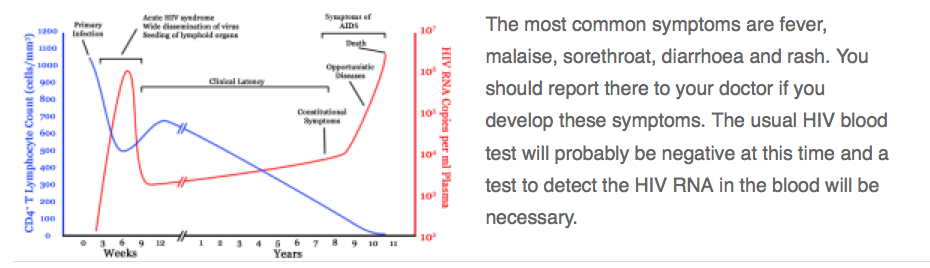 For how long should I continue PrEP and how do I stop it? You should continue to take PrEP daily for as long as you are at risk. If the situation changes and you are no longer at risk, continue PrEP for one month from the last sexual exposure. ARV pills truvada atripla Where can I get additional information on PrEP? More FAQs are available at prepfacts.org/the-questions http://www.cdc.gov/hiv/pdf/PrEP_fact_sheet_final.pdf |
| Advert Space Available |
 |
| Bookmarks |
| Thread Tools | |
|
|